Understanding Mobility
Mobility is one of the concepts of fitness thrown around with a variety of descriptions, means, and methods for improving or using it without understanding whether that improvement is necessary or even possible. One potential definition of mobility is the available range of motion of a joint in a specific direction. Another is the available and usable range in a specific movement. Another is a global ability to move through a range of motion. Yet another could be the length of a muscle. These can all have similarities, but are in themselves very different from each other.
Joint mobility as defined by most medical dictionaries is the ability of a joint to be moved through its range in different planes. This is dependent on the characteristics of the individual joint itself as well as the supporting muscles and ligaments,the capsule and the anatomy of the articulating surfaces.
Flexibility or limberness as defined in most common dictionaries refers to the absolute range of movement in a joint or series of joints, and length in muscles that cross the joints to induce a bending movement or motion.
Both of these definitions could define what is also known as passive range of motion, or what is accomplished with minimal feedback from the individual and not subject to their conscious cues. Active range of motion is how much range the individual can move their limbs through with conscious commands. For instance, if I assess someone’s hamstring flexibility with a passive straight leg raise, I’m looking at how much range of motion they have through their hips in flexion. An active version is having them raise their leg up to see how much flexion they can use on their own in that direction without outside assistance.
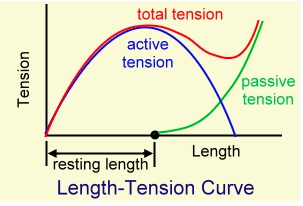
In many instances, the passive range of motion achievable in any joint will be greater than the active range of motion that could be achieved. Much of this is due to the limited contractile ability of any muscle in it’s most shortened position.
You can see that active tension drops off significantly before the end of the available length of the muscle, and that the remaining tension applied in the joint is due to stretch through the ligaments and joint capsule, not necessarily through the muscles that would move the joint into that position in the first place.
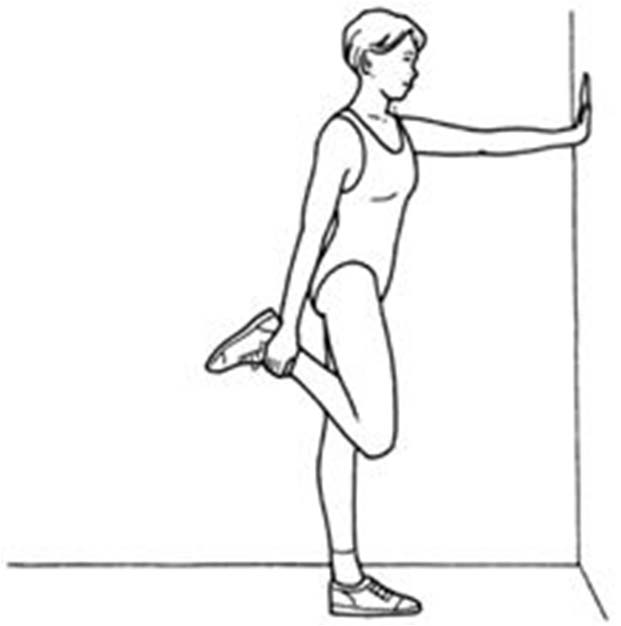
There’s also the concept of insufficiency to get into this position, usually mediated by either passive insufficiency or active insufficiency. In passive, you just don’t have the length to allow entry into that range of motion. For example, trying to do a straight leg flexion compared to a bent leg flexion. If the straight leg is reduced but the bent leg raise is huge, there’s likely a passive insufficiency through the posterior chain muscles of the low back, glutes, hamstrings, and calves. An active insufficiency is an inability to produce muscle force to enter into that length. Another example is using a knee flexion mode for something like a quad stretch. A passive insufficiency would mean you couldn’t grab your foot and bring it to your butt because something’s resisting it.
An active insufficiency would be an inability to contract the hamstring to replicate that position effectively, or at least get close to the passive component.
In this example if I’m able to get my heel to my butt (I can) but I wind up actively only using this much range, there’s an insufficiency of about 30 degrees. If you want to try this out, get ready for some life altering hamstring cramps on the first few go arounds.
So far we’ve only looked at the potential range of motion available with no influence of outside variables. I’ve talked about potential structural limitations to range of motion before, so I won’t go into much more detail here. Instead of looking at the hardware aspects of mobility, let’s spend some time looking at the software. The brain and peripheral nervous system is one of the largest determinants of mobility there is, and understanding it and using it effectively can be the difference maker in having a mobility program that works and one that doesn’t.
The brain controls both conscious and subconscious muscle tension and reflexive contraction and relaxation. In patients under anaesthesia, some studies have shown immediate increases in joint range of motion once neural input is removed. Cerebral palsy commonly comes with hemispheric muscle spasticity, meaning the muscles are chronically “turned on low” and in a shortened position. A condition known as heterotropic ossification develops on the affected side of people with hemispheric cerebral and cerebellular disturbances, but not on the unaffected side, and winds up reducing range of motion through those affected joints significantly.
Coma patients, even the very elderly and degenerated, can commonly have massive joint ranges of motion through their hips and spines with zero neural input in to them. Paraplegics can suffer from contractures, which is a shortening and fibrotic stiffening of the muscle tissue with disuse and seated postures, but can still have spasm contractions from the muscles in response to changes in joint angles and velocities. Occasionally these spasms are oscillating wave-like spasms or twitches that increase and decrease in both amplitude and frequency, and sometimes they’re just consistent twitches for a few seconds or minutes, and others can be full on tetanized contractions that last for a long time.
https://www.youtube.com/watch?v=YkBX6VbdjV8
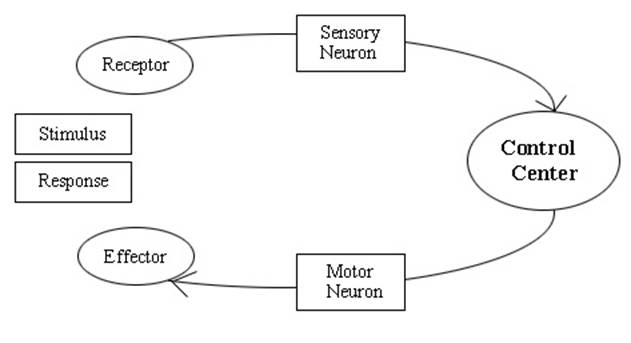
These spasms are entirely devoid of central input and are likely due to spinal reflex loops that cause the muscles to contract in response to something. A classic example of these spinal reflex loops is the knee jerk response to tapping the patellar tendon with a rapid force, as used by doctors with a rubber mallet to test reflex speed.
We can work off of these spinal reflex loops to create increased or even decreased mobility in the entire body.
This increase in neural drive in a protective manner caused a reflexive relaxation following the activity, which helped to increase range of motion. It also helped reduce protective guarding by increasing muscle activation around the spine.
A similar reaction to increased neural stimulation can be seen here, where scraping the masseter in a painful manner causes a big spike in neural impulse through the entire body, and removal of the stress caused a reciprocal reduction in protective tone, sort of like when a massage therapist digs into a tight knot and when they’re done you feel more relaxed.
https://www.youtube.com/watch?v=B4ZPfOHjYiI
The muscle being worked on itself wasn’t the keystone to producing new range of motion, but the systemic application of a neural stressor that the body had to adapt to, one way or another.
This is one of the main outcomes of the autonomic nervous system, the “fight or flight” system that causes increases in neural, endocrine and cardiac outputs to help you respond to stressful stimuli to help you either defend yourself or run away from trouble. If you’re in a ready and low anxiety state, your passive and active range of motion will be better than if you’re in a stressed out or anxious state. Here’s an easy video demonstration:
The pulsed breathing increased neural drive and produced a state of heightened awareness in a “ready” mode, which is essentially the goal of any warm up or preparation used by elite athletes, even if not using this exact technique. Slapping the shoulder produced a noxious stimulus that made the body think something was wrong, and the response was to tense up to produce more muscular force or twitch response if he had to roll or run off the table in response to the stressor.
Some people can be in a near constant state of sympathetic stimulation, always on edge or exhibiting more anxiety to states of arousal compared to others. They may constantly tap a toe while sitting or fidget excessively, but relaxing is somewhat difficult. In studies, those who had higher than average sympathetic drive also reported an increase in tendinous pain response. This could maybe be due to consistently having tension run through the tendon and receiving little time for recovery and positive adaptation, or maybe they’re hypersensitive to their environment. Either way, it’s an interesting connection.
In my experience, the people who could be said to be more sympathetic dominant or “on edge” tend to also be much tighter and respond poorly to both active and passive mobility techniques. They do tend to have a resting tension that can make them more elastic, which makes them decent at distance running and relatively unbreakable in some ways.
Activities that promote more parasympathetic stimulation also tend to produce range of motion increases compared to control. Yoga, tai chi, qui gong, and meditation all use methods of breathing that have been linked to parasympathetic stimulation, and these breathing techniques are also favoured by dancers and gymnasts to get into very deep stretches.
The main method of consciously stimulating the parasympathetic system is through long, slow and deep breathing, both inhaling and exhaling. Think of taking 5 seconds to inhale, long and smooth, and then exhaling for up to 8 seconds per breath. The exhale is more of a release than an expulsion of the air. Doing this breathing for a minute or two can have massive effects on neural drive through the body, and also on mobility.
Try this out. Stand up, and try to touch your toes with straight legs. See how close you can get. If you’re already on the floor, just sit off to the side and let the tight kids have some fun, okay? Next, try to take 5 long slow breaths as outlined above, and then try to redo the test and see what happens. Odds are, you’ll increase the range of motion you’re using.
Some tools can be used to measure neural stimulation and whether it’s a chronic thing or not. Heart Rate Variability has become very popular, but one downside I would suggest is it’s something that has to be tracked over time to see a specific difference. It’s not as reliable to see a difference through the same day, and even in response to individual variables like a training set, or a different environment itself.
I would propose that a device to measure respiration rate and also respiration variability would be a good way to measure autonomic nervous system activity. A chest strap monitor with a force coupler that could measure rib expansion and compression, and also the rate of both to see if they are smooth and linear or short and choppy, would likely give a better idea of whether someone was in more of a sympathetic state or parasympathetic state, and also provide more real time updates at that moment. If anyone’s reading this who can make something like this happen, my finders fee is 10% of all future revenue 🙂
For the vast majority of treatment modalities designed to see increases in range of motion of a tissue or joint, much of it comes from alteration of the neural input to the tissue. Techniques like ART or Graston use friction and mechanical stimulation to produce change through irritation of the tissues. I’m not aware of any research or histological explanation of how these techniques can actually break up scar tissue or adhesions, but they do seem to follow the concepts of neurophysiology outlined above.
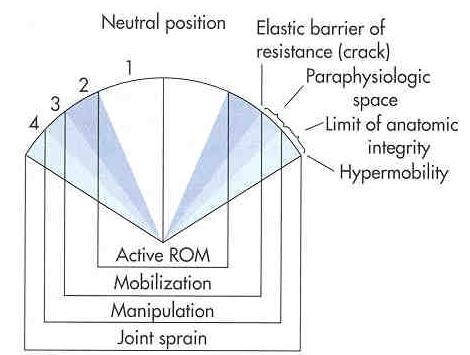
Other techniques like dry needling or acupuncture work on stimulating myoreceptors to induce a spasm response and again alter the neural tone of the tissue. High velocity low amplitude (HLVA) adjustments common in chiropractic treatment do something similar by rapidly altering a joint position and causing a proprioceptive response in the tissues. One criticism of this approach would be that the adjustment in the absence of some form of motor pattern re-education may be a limited benefit to the patient as the proprioceptive elements can just go back to where they were before, leaving them tight again in a couple of hours.
Actively breaking up scar tissue tends to take considerable force and recovery modalities, like manipulating a total knee replacement under general anaesthesia to restore post-surgical range of motion if the individual didn’t maintain mobility and activity.
In about 1.3-13.5% of patients who receive a total knee arthroplasty, they may see significant and painful reductions in joint range of motion due to operative scar tissue formation, meaning they have to undergo a manipulation under anaesthesia. You could imagine the process would be pretty painful, which is why it’s done under anaesthesia.
This scar tissue reduction is not something that can easily be addressed with a tool assisted therapy, but realigning scar tissue fibers themselves can be assisted with different tools and force applications. By working the joints it can help to reduce the haphazard manner of scar tissue formation and make the fibers of collagen line up more with the directions of force application, meaning range of motion is usually maintained.
Now let’s say you’re one of those fun folks who has tight joints, early bone to bone contact within a range of motion, and physiologically “short” muscles when stretching. These are all considered to be structural restrictions and don’t easily respond to neural aspects of mobility training. Can something still be done? Sure, but you’re not going to easily enjoy it.
Many dance and gymnastics coaches rely heavily on static stretching for their athletes, and in some cases require those stretches to be held for 10-30 minutes at a time. That’s right, by the time you start your stretch to the time you finish, Alex will have gone through Jeopardy, Double Jeopardy, and then Final Jeopardy before you’re able to relax out of that bad boy.
Most gymnasts begin training when they’re very young as their joints and capsules are incredibly tolerant to stressors and they can get much more mobile young than they can old, which is why many of them will retire by the time they’re 17. If you were able to be very mobile when you were young, there’s a much better chance of being mobile when you’re older, and especially so if you can pass basic hypermobility testing like the girl above.
You can see similar remodelling of the bones lining a joint, the joint capsule, and the surrounding soft tissue with consistent force application and remodelling. That’s one of the benefits to cells such as osteoblast, osteoclasts, myoblasts, myoclasts, and satellite cells is they have the ability to remodel damaged or used tissues to adapt them to the stressors applied.
One note of caution though is this remodelling can be beneficial or detrimental depending on the amount of force applied. There’s always a threshold for good stuff to happen and where more of this turns in to bad stuff. If too much stretch loading is applied to muscles, tendinopathy could result. If too much compressive loading into bones is applied, bone spur formation could result. If on the hips or shoulders, it’s called impingement, and may need to be removed surgically to restore range of motion. Each person will have a different threshold, so tread lightly.
So in terms of what could influence mobility, I’ve managed to outline structural variations, neural drive and other aspects of the nervous system, as well as age related decreases in motion. The last one can be offset by simply staying as mobile as possible for as long as possible. I have a 74 year old client who can still squat to the floor on command, simply because he squats every day. I have 30 year old clients who can’t come close to this.
Next, let’s look at how much mobility you actually need and what to do if you don’t have enough.
I’ve always liked making assessments as simple as possible and determining what I can do with someone from the basics. Essentially, if an assessment tells me a person has enough mobility and control to perform a litany of exercises, I don’t really need to get more specific than that in most cases.
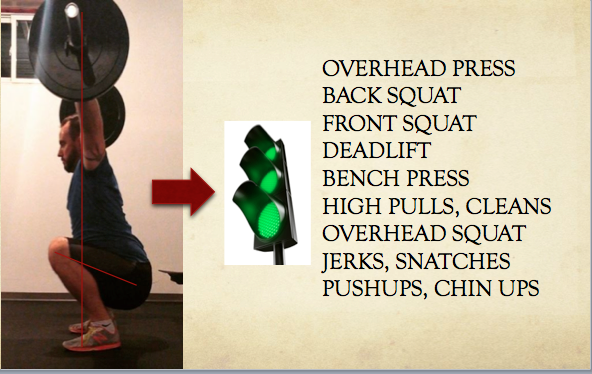
A great example is a basic overhead squat. If someone can nail an overhead squat out of the park, they’re pretty much showing you that today they have the ability to do a bunch of exercises with no further intervention required.
They may not have the skills in these exercises yet, but they’ve shown they have at least the fundamental physical aptitudes to do them. I can coach the rest.
If someone can’t do this, then we can start drilling down to find out whether it’s an issue with strength, control or specific mobility if needed, and then determine where we have to work. Essentially, if they have enough mobility to do what I’m looking to have them do to achieve their goals, it’s enough mobility. If they don’t have enough to do the things they need to do or want to do, they need to work on improving their mobility.
Consider it another way. If you want to take a trip and the plane ticket costs $5,000 and you only have $3,000, you need more dollars. You don’t have enough to do what you want to do. If you have $6,000, you don’t need more dollars. You have enough and then a little cushion.
If you want to squat below parallel, your hips should be able to flex to at least 110 degrees. If you can’t do that, you need more hip flexion mobility. That makes sense, right? Anything more than that is just icing on the cake in terms of what you have compared to what you need.
You technically only need to “work on mobility” if you’re deficient in some way or simply want to maintain what you have. If you want to do more and explore a larger range, you can absolutely work on that too, and if you want to keep up with some of the flexible Gumbi’s on Instagram, you’ll have your work cut out for you.
Now assuming you have no real structural issues that would automatically prevent you from doing something about improving your mobility, let’s look at some methods you can use to help get you somewhat more awesome at putting your foot in places feet shouldn’t go.
First, you have to look at what joints, positions and movements you want to improve. This is a big part of the process as simply thinking I want to globally move better and with more mobility is a big goal, definitely hittable, but huge nonetheless. It often starts with picking your parents a little more wisely. Start small and pick one thing to start on.
When doing any mobility drills, there’s a specific consideration to how you’re breathing, as that will be what dictates whether you’re using sympathetic or parasympathetic activation, and how readily you can achieve the changes in joint position accordingly.
There’s a definite hierarchy to techniques you can use to improve mobility, and it goes like this from systematically easiest to hardest:
- passive static stretches
- static eccentric positional holds with antagonistic contraction
- static eccentric positional holds with antagonistic and agonistic contraction
- dynamic range eccentric training with antagonistic contraction
- static concentric positional holds
- dynamic concentric resistive positional holds
Let’s use hip flexor stretching as an example for these.
Passive static stretches are a mode everyone is familiar with. You lean into your hip, pushing it into extension and stretching the hip flexors through bodyweight tension.
Lean into the muscle until you feel a stretch, and then just hang out for a few minutes, trying to breathe deep and long as described earlier in the parasympathetic section.
Static eccentric positional holds with antagonistic contractions are a little more complex, but not really. In this example, you would do the same position, but then try to contract the muscle that would push you further into the stretch or that would oppose the muscle you’re stretching. In the instance of the hip flexors, that would be the hip extensors. Try to contract your glute on the same side of the hip hard, and drive deeper into hip extension.
This contraction can be completely adjusted by simply ramping up or down the intensity of the glute contraction. You could easily make someone sweat bullets and even pass out from a simple hip flexor stretch if they made the glute contract hard enough, so it can be a workout in itself.
When doing these, breathe deliberately, big forceful pull in, and hard exhale out to try to increase neural drive to the contracting muscles.
Static eccentric holds with both antagonistic and agonistic contractions is a cycling contraction where you breathe in and try to pull the stretched muscle into a shortened position (hip flexion in this case) and then breathe out and try to fire the antagonistic muscle into it to create a new range of motion (the glutes in this case). Again, breathe deep and modify based on intensity of contraction.
Dynamic range with antagonistic contraction is more of the active mobility drills with some of the extra firing of the glute at the end of the movement. An example would be a split squat with hard effort from the glutes.
Note the High Tensile Strength t-shirt in the video.
Another option could be agonistic contractions as well, like a standing hip flexion using band resistance.
For each example you’re breathing out fully and with force during the concentric or contracting portion of the movement.
Static positional holds involve actively pulling a joint into position using the muscles involved in the process. A solid example of this would be simply trying to flex the hip and hold on to a shoe or ball or something, and then trying to generate enough tension to crush the sucker.
Breathing on these is forced and high tension, with long inhale and long exhale, and lots of pressure behind them.
Dynamic concentric resisted holds would be something similar, but then increasing tension against some form of resistance, like wrapping a band around your foot or hanging a kettlebell off that sucker. Either way, it means adding load to the area.
There’s a ton of options when it comes to increasing usable range of motion, And they can all produce some benefits in one way or another.
One thing to consider when looking to increase mobility is how you feel and what that feeling might mean in terms of whether you need more stretching or more contracting. There’s a lot of people who will say they “feel tight” even though they spend a lot of time stretching and have really solid mobility. This could be in any region of the body, but I find if someone has had an injury they’re especially aware of whether they feel tight in an area and almost habitually self-assess and stretch. The low back is common for this.
If the person feels tight but is constantly stretching and has great overall range of motion, they aren’t actually tight but more their backs might just be experiencing some increased neural drive from them being hyperaware of the area. It’s almost like a self-fulfilling prophecy when the person pays so much attention to the area that it leads to the muscles feeling tighter, without shortening the muscles at all. They might also confuse this tight sensation with pain, so understanding the differentiation can be a major obstacle to get through.
Another form of tight is a muscle soreness following a workout, sort of like delayed onset muscle soreness (or DOMS). This is something that typically gets better with more movement and isn’t a big issue. You’ll likely find after doing some of the active mobility drills listed above that you’ll get some significant DOMS the day after. That’s okay, but can still lead to a feeling of tightness in the muscle.
Another “tight” is trying to access a range of motion that you had previously been able to get to but today for some reason it’s harder to get there. So involving some of the active mobility drills above will restore it pretty quickly.
So to recap, there’s a lot to consider when it comes to improving mobility, starting with whether it’s actually necessary at all and in what directions would you see the best benefit. If it’s structural, you’re going to have a hard, long time trying to get small increases in any range of motion, and less so if you’re older than if you’re younger. If it’s not structural restrictions, it’s likely involving the nervous system in some way, so then it’s a matter of trying a few things like breathing drills or the active series I outlined earlier to see if either provides any benefit in a tangible way.
If mobility doesn’t improve on your own, it could be time to get some therapeutic intervention through some tool assisted modality, adjustment, or whatever else you feel resonates with your thought process and comfort level. If those don’t work, it’s likely a structural restriction at that point, so circle back and go slow.
If all you want to do is daily life and train common exercises in the gym, you’re more than mobile enough if you can squat low, touch your toes with straight knees, and put your arms over head with your biceps touching your ears. If you can’t do those, start with the goal of improving those outcomes and you’ll be set.
If you have sport goals in mind, much of your mobility requirements will be dictated by the goal activities. Focus on whether you have trouble doing specific activities and try to work on improving mobility relative to those activities.
Hopefully this outline helps people form better ideas of how to approach their mobility, and also help to understand if they actually need to work on getting more or not. Enjoy!






6 Responses to Understanding Mobility