Vitamin D: 3 Things You Probably Know, 3 Things You Probably Didn't
In part three of their epic series, Sol and Kurt from Examine.com are back. This time they’re dropping K-bombs on one of my favourites, Vitamin D. Seeing as how Edmonton gets sunlight for roughly 5 months of the year (February not being one of them), supplementation plays an even more crucial role.
If there is any supplement that gets recommended by everyone, it’s Vitamin D.
Similar to our previous guest posts on creatine and whey protein, we cover three things you likely knew, and three things you likely did not:
Three Things you Probably Already Knew
Vitamin D helps aid in skeletal mass preservation and reduces falls in the elderly
The ability of Vitamin D to enhance skeletal mass and functionality in the elderly is well known, and is one of the more commonly touted claims behind Vitamin D. In a sense, elderly persons who have a deficiency of Vitamin D (or at least bordering the deficient range) who then supplement with 400-800IU or more of Vitamin D appear to have a reduced risk of falls and subsequent injury or hospitalization.
This seems to only affect those with Vitamin D deficiency, with additional Vitamin D to bring one past a normal range or supplementation to people with already sufficient Vitamin D status not conferring additional benefit to risk reduction. Taking additional calcium supplementation alongside the Vitamin D confers a bit more protection in those deficient in Vitamin D, which are usually elderly women at risk of osteoporosis.
Dean: Or Gwenneth Paltrow. Seriously, she was diagnosed with osteopenia, yet insists her trainers’ requirement of never lifting anything more than three pounds is keeping her healthy.
This fact of Vitamin D is actually the most socially important aspect of Vitamin D as it has direct ties into reducing mortality/morbidity and improving quality of life in a cohort that is commonly not targeted by producers of supplements.
There really isn’t that much evidence to support an increase in testosterone
We cannot say that Vitamin D doesn’t increase testosterone, but will say that currently the entire body of evidence in support of Vitamin D increasing testosterone involves a study in men that lasted a year in length using just over 3,000IU Vitamin D; this study was in diabetics and they did not actually intend to measure testosterone but noted that it was significantly increased in a male subset, so they made note of it and published it.
It most likely does have a role in increasing (or at least preserving) testosterone levels, but it currently isn’t a really well proven intervention or anything. Currently, we just have preliminary evidence that having serum Vitamin D over 50nmol/L is probably better than having lower levels in regards to circulating testosterone and free testosterone.
Vitamin D has not yet been shown to do much for fat loss
With the popularity of Vitamin D on the rise, why not just outright claim it is a panacea and does everything? It increases testosterone and improves male fertility, so why not say it makes you shredded as well?
Unfortunately, all claims to suggest that Vitamin D has fat burning potential are currently unsupported or at least very preliminary. There is definitely a correlation between low serum Vitamin D concentrations and obesity (particularly childhood obesity) and it is theoretically plausible that it may reduce fat mass in clinically unhealthy persons (current school of thought is directed at a reduction of adipose tissue inflammation) but this is currently unsupported.
Three Things you May Not Have Known
The link between Vitamin D and Longevity is quite conflated
Usually when a supplement is touted to increase lifespan, it is thought that it tends to work by either somehow acting on genetic factors to promote an empirical extension of the amount of time until you die (currently, no supplement is well supported in humans for this) or at least reduce the amount of premature deaths in older persons merely by being healthy; the reduction of death, usually via cardiovascular support, manifests itself as an indirect extension of life (curcumin and resveratrol, as well as green tea consumption and moderate alcohol consumption, seem to work via this manner).
Vitamin D does appear to empirically extend the average lifespan in human with adequate serum Vitamin D concentrations in serum relative to those with deficient levels.
This seems to be due to less falls in the elderly, for the most part.
For those unaware of exactly how severe ‘falls in the elderly’ can be, when skeletal muscle and bone are in a weakened state such a fall (given some prior conditions being met) could result in bone fracture; the bone fracture itself is nonlethal most of the time, but the subsequent hospitalization paired with a poor immune system could result in lethality secondary to infection. Due to this surprisingly common sequence of events, preventing elderly persons from falling works to increase lifespans.
As such, Vitamin D supplementation seems to be associated with longer lifespan secondary to less falls in the elderly as mentioned earlier. Although interactions between Vitamin D and telomeres (thought to be indicative of lifespan) have been studied, there is currently not enough evidence to support a true life extending property of Vitamin D.
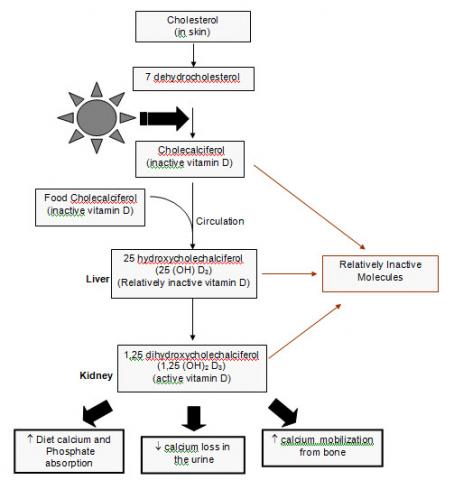
Vitamin D involves an active hormonal form and inactive prehormones
Whether you decide to supplement with Vitamin D2 or D3 (the latter being seen as ‘better’ due to superior absorption), these are for the most part inactive prehormones; the Vitamin D that acts in the body is indeed an active hormone, and has its own receptor expressed on the cell nucleus and cytoplasmic membrane that mediates most Vitamin D-like effects.
Vitamin D3 is also known as cholecalciferol, and needs to be hydroxylated (an addition of a hydroxy group) at ‘stage 1’ and ‘stage 2’. Stage 1 is commonly thought to occur in the liver (into 25-hydroxycholecalciferol), and Stage 2 is thought to occur in the kidneys mostly (1,25-dihydroxycholecalciferol). Once these two hydroxy groups are added, Vitamin D is in its active hormonal form.
It should be noted that the enzymes that mediate these effects are expressed in a large amount of tissues and even immune cells, so production of active Vitamin D is not wholly localized despite traditional thought.
This bioactivation is also a reason why superloading 100,000 IU of Vitamin D at once won’t kill you. The amount of active hormonal Vitamin D you are actually getting is limited due to the enzymes that mediate hydroxylation having a rate limit associated with them, despite a massive surge of cholecalciferol in your body now (which is referred to as your ‘Vitamin D status’)
Vitamin D appears to be one of the only potential treatments or preventative health medications for Multiple Sclerosis
This claim is highly interesting as it was first discovered secondary to a high correlation between multiple sclerosis risk and latitude (which we now know is more related to sun exposure, as it seems to hold across cities and cultures) and later studies implicating sun exposure per se. There is strong evidence to suspect a link between the sun and its exposure and reducing the risk of MS.
So far, preliminary studies using Vitamin D seem to replicate the observed protective effects in rodents and may actually synergistically augment the standard MS therapy (interferon beta) and are thought to be protective at the level of the neuron. This is important to note as although there is a strong link to sun exposure, Vitamin D may not be the only thing that is made in the body via UV radiation (definitely the most studied of course).
When it comes to over the counter options to reduce the risk or try and prevent Multiple Sclerosis, Vitamin D is pretty much alone. There are not many options for MS prevention, so seeing the preliminary evidence turn up positive has been talked about a lot in the media and is getting a deserved amount of attention.
Our Vitamin D page has over 250 citations if you want to learn more.
Sol Orwell and Kurtis Frank are co-founders of Examine.com, a science-based compendium on supplements and nutrition.


3 Responses to Vitamin D: 3 Things You Probably Know, 3 Things You Probably Didn't