Training The Hypermobile Client
There’s a big difference between someone who seems to have a lot of available mobility and someone who has an actual diagnosed hypermobility issue due in some part to wonky connective tissue production or repair.
Here’s a brief chart on some of the potential connective tissue disorders that can impact collagen and elastin synthesis and repair, with hypermobility issues on the left and limited or restricted issues on the right.
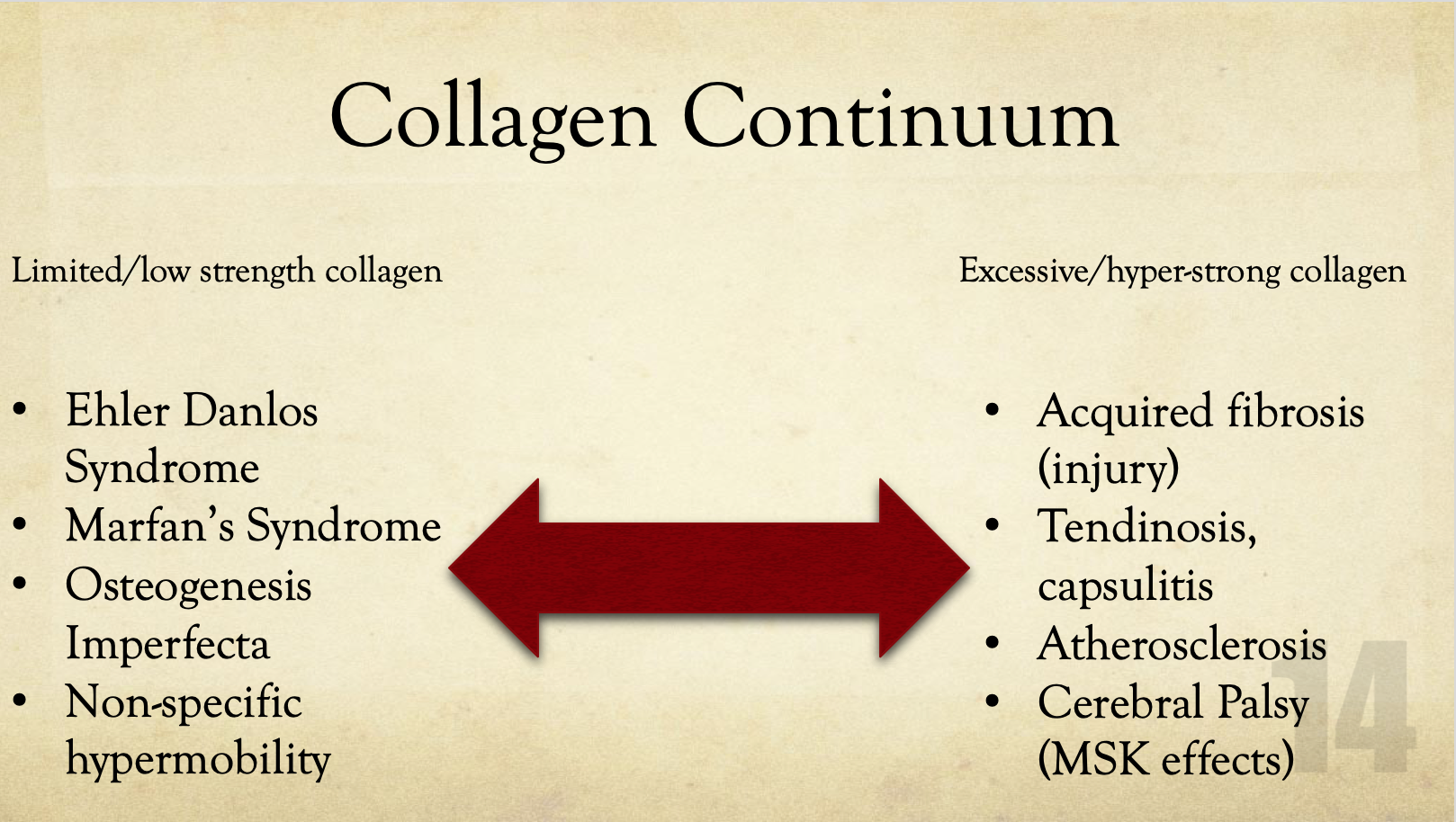
In each of these scenarios, it could be a continuum as well, with someone diagnosed with, say, Ehler Danlos having only minor symptoms that are easy to control and someone else with the same diagnosis being very much incapacitated by it. Conversely, you could have someone who has hypermobility tendencies that can acquire joint stiffness from some source of injury.
My wife dislocated her elbow this summer, and while she tends towards non-specific hypermobility based on a 9/9 score on the Beighton Laxity Score, her elbow became fibrotic, requiring about 12 weeks of progressive splinting to recover the range of motion.
If someone has an issue producing or repairing connective tissue, it tends to go beyond simple muscle and tendon function, and can impact stuff like digestive system function, skin, hair, reproductive tract health, and essentially anything and everything that involves some level of connective tissue strength and resiliency. Off-hand, a client who is an orthopedic surgeon who specializes in hip and knee replacements told me that hypermobile patients tend to need joint replacements at an earlier age than patients who aren’t hypermobile, which lends to a couple of possible theories.
Think of someone who has general hypermobility due in part to reduced collagen strength or production as akin to winter tires for your car. If you live somewhere where snow only exists on Instagram, this analogy won’t really work all that well, but just nod along until everyone else is done. The rubber on winter tires is softer, and allows for better grip in winter driving conditions compared to summer radials or all seasons. This allows better traction, but because it’s a softer rubber, it wears down faster, typically by anywhere from 10,000 to 20,000 miles sooner than similar all seasons.
Similarly, if someone has weaker or “softer” collagen than someone who isn’t hypermobile, it stands to reason that it would be less resistant to stress comparatively, and would also wear down at a faster rate than someone who has higher strength connective tissue.
Black et al (2008) found that with increasing ratios of collagen to elastin, extracellular matrix sheets tolerated a greater strain compared to sheets with lower concentrations of collagen and compared to elastin only.
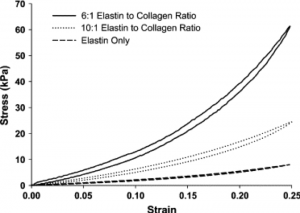
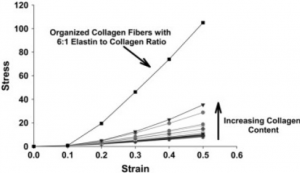
In these graphs, stress is the amount of force applied to the tissues and strain is the relative change in length (stretch) the tissues go through. A higher relative stress to strain relationship means the tissue is stronger and can tolerate external forces more easily with less damage. Conversely, a lower stress to strain relationship means the tissue can deform easier, much like blood vessels that have to respond to rapid changes in blood volume and pressure without damage.
Stronger connective tissues with higher collagen to elastin ratios is great to have in places like tendons, ligaments, meniscus, joint capsules, and fascial sheaths, whereas more maleable connective tissues work really well for stuff that needs to stretch and respond more rapidly and frequently, like blood vessels, skin, digestive tract, and similar regions.
If someone has a tendency towards hypermobility, this can mean their joints are more prone to early degenerative changes versus someone who is generally less likely to be hypermobile. This is even more prevalent among diagnosed connective tissue issues, and something to seriously consider when starting up in a strength training program.
Interestingly, wear and tear in these instances does not necessarily equate to greater levels of use. Dr. Craig Liebenson recently put up an amazing post on Instagram outlining some of the research regarding marathon running and relative rate of osteoarthritis development in active runners knees and hips.
Now part of this could be self-selection bias. People who have joints that can tolerate the pounding of running tend to enjoy running much more than someone who has very limited joint stability and who wind up wearing down their active support system more quickly, so the people built to run, run, whereas the people who aren’t, don’t.
But it could be theorized that people who are good at running marathons have summer tires for knee menisci, and wear down at a slower rate than people who aren’t so fortunate.
Another concept to consider aside from simple wear and tear when dealing with hypermobile individuals is their rate of recovery can be significantly impaired compared to someone who doesn’t have those same issues. Because their connective tissue may be less stiff, and remodelling rates could be longer due to impaired production or regeneration, training volume, frequency and recovery times may be affected.
If Person A has a higher ratio of collagen to elastin than Person B, they can likely bounce back from a hard training session relatively quickly and put up some solid workouts within a single training phase without any issues, whereas Person B may feel soreness for a little while longer following a hard workout, and may have a higher incidence rate of overuse injuries like tendinitis, bursitis, plantar fasciitis, pinching hip syndromes, cough due to cold, ebola, or a bad case of taco-induced itis.
The challenging part about the above scenario is that it’s entirely individual and difficult to determine where the threshold for what the person can tolerate in terms of balancing intensity, volume and recovery, until they start to become symptomatic. That may be after the first workout, or the 50th, or anywhere in between. It can be a negative cycle of train, flare up, recover, back to train, and flare all over again. This can be frustrating to anyone, let alone someone who just wants to train and feel good.
If you suspect yourself or someone you’re working with has more of a hypermobility tendency, it would be very beneficial to use volume and intensity in more of a wave manner with periods of higher stress and phases following for recovery with lower intensity and volume, or by including dedicated deloading phases to ensure tissues have a chance to recover from the work they’re going through and prevent inflammatory responses from overuse.
Let’s look at a classic example of a 4 day a week program.
Now, 4 days a week may be easy enough to manage for many, but with back to back days at least once, and often only one day of recovery between workouts, for someone who is hypermobile it may be more frequency than they can effectively recover from, even if matching intensity and volume within a workout.
So instead of a schedule like Monday, Wednesday, Friday and Saturday to hit all 4 days, it may be necessary to follow less of a 7 day calendar to hit all 4 days, and make more of an 8 day training “week.”
For instance, this would involve workouts on Monday, Wednesday, Friday, Sunday, and then repeat on Tuesday, Thursday, Saturday, Monday for week 2. This one extra day each “week” expands the recovery time available and reduces the overall systemic stress compared to a 7 day week.
It may also work better to reduce frequency from 4 days a week down to 3 in many cases. I’d rather have a client feel good with a lower freqency and thus put out better quality training than always feel beat up with a higher frequency.
Phasing volume each week could be another approach. Let’s say your average volume for a week of 4 days a week of training was something like 80 sets of work (20 sets per workout, 4 workouts a week). Assume intensity is matched. So in week 1 you do 80 sets, week 2 you do 80 sets, week 3 you do 85 or 90 sets, and week 4 you drop down to 60 sets as a recovery week. You can live your best life at 80 sets a week, but anything over that makes you feel a bit like your soul is being crushed, so the training stimulus is very short with a recovery phase built in behind that. to help get back to baseline before the following phase begins.
You can do something similar with intensity, using Rate of Perceived Exertion (RPE) or Reps in Reserve (RIR) as metrics for overall intensity compared to just percentage of 1 rep max being lifted. If I do a set of back squats and at the end I say that felt like an 8/10 effort, whereas 1 is being conscious and 10 is being chased by a bear, while on fire, and the bear is on fire, and everything is on fire, and I’m trying to run so hard the wind from my running is the only thing I have to put out the fire and I have to run faster than the fire bear if I want to see tomorrow.
RIR is more about how many more reps I feel I could have done at that specific load. I finish a set of 5 reps with 315, and when I rerack I feel confident I could have still mustered 2 more reps, then my RIR is 2 for that set.
So for someone with hypermobility, we may need to program more sets at a sub-max intensity, around a 6-7/10 RPE, or an RIR of more than 3 for most exercises and most weeks. Occasionally we can drift into higher loads and intensities, as long as the volume stays low and recovery stays high.
Again, these are all very broad recommendations, and each person will respond to training in entirely individualized ways. Some may tolerate more loading intensity and volume, while others can do one rep and feel like everything is dying on the inside. Because of this, the programs should be very much geared towards some level of autoregulation where it can be changed on a day to day basis based on how the person is feeling, and whether they’re getting any overuse symptoms popping up.
There aren’t any special exercises or tricks to help train people with hypermobility, just understanding how to work within their means and seeing steady progress like with anyone else. Much of the big challenges to training hypermobility are difficult to see, and depend on communicating how that person feels following a workout and if they’re getting any undue soreness, then adjusting the program accordingly. Progress slowly, stay patient, and work as hard as they can tolerate, and you can have some big success.