A More Sophisticated Approach to Correcting Knee Dysfunction
Today’s awesome guest post comes from Brent Brookbush, DPT, a physical therapist from New York who has an amazing resource for trainers and clinicians to learn more about anatomy, corrective exercises, and a bunch of other golden goodies. Plus, he’s included a special offer but you’ll have to read the article to find it.
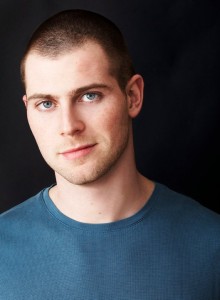
By Brent Brookbush, DPT, PT, MS, PES, CES, CSCS, ACSM H/FS
President of the Brookbush Institute of Human Movement Science
Join BrentBrookbush.com to access all of our online content!
Get DeanSomerset.com Discount Codes Below!
*****
In my humble opinion, the knee is a “victim joint.” That is, the knee is rarely the source of dysfunction, but rather the unfortunate victim (often painfully so) of alterations in hip and/or ankle motion. The knee is just the “monkey in the middle”.
Vastus medialis obliquus (VMO) strengthening has been the “go-to” intervention for improving knee pain, dysfunction and pathology, but I believe there is a growing number of human movement professionals (PT, DC, ATC, LMT, CPT & SC) who have been disappointed with outcomes from this intervention alone. Further, many compelling arguments have been made regarding the practicality of VMO activation. For example, can we truly isolate the VMO from the other muscles of the quadriceps? And, why would you squeeze a ball between your knees to activate the VMO when this may also increase functional knee valgus and contribute to further dysfunction?
By no means is this article meant to discourage human movement professionals from increasing quad strength, especially at the end-range of extension. However, evidence is building for a more sophisticated approach to this issue, with the potential to optimize movement patterns throughout the lower extremity, increase performance, and decrease our risk of injury.
Excessive Internal Rotation and Adduction of the Hip:
Studies examining individuals with patellofemoral pain syndrome, iliotibial band syndrome, ligament rupture, and even achilles tendinopathy, most often present with excessive hip internal rotation and adduction moments, commonly observed as “knees bow in” (a.k.a. Functional Knee Valgus) during functional tasks1-9. Based on this research, there are multiple factors contributing to this “excessive” internal rotation and adduction, and MULTIPLE FACTORS IS A GOOD THING. Anytime you see multiple factors contributing to a dysfunction do not think “WOW that’s complicated”, instead think “look at all the potential issues I could address”. More factors could mean more potential interventions, which could mean more opportunities for success.
Some of this research suggests weakness, latent firing, and alterations in motor control of the gluteus maximus (GMAX) and gluteus medius (GMED)4, 7, 10, 18. The eccentric function of the GMAX and GMED is eccentric deceleration of adduction and internal rotation, so, inhibition of these muscles should come as no surprise; but, it is always nice to have a little research to back our logical assumptions. These findings are a huge plus for practical application, as we may not be able to do as much as we would like about VMO activation, but glute activation, we can handle that (discussed below)!
Some studies related to knee valgus also imply over-activity of hip adductors10-11, indicating that release and flexibility techniques may further assist in optimizing movement patterns. Again, this is a big win for practical application. Downside, these studies did not examine the over-activity of hip internal rotators (except for the adductors). This is surprising in the case of the tensor fasciae latae (TFL), which is a strong and superficial internal rotator of the hip. Two studies have noted increased TFL size and activity in the presence of hip dysfunction13,14. Although this is not direct evidence that TFL over-activity contributes to knee dysfunction, this evidence may be worthy of assessing the TFL during practice.
One area that needs further study is the effect of excessive internal rotation and adduction on arthrokinematics (effects on glide and roll) of the hip. It has been theorized that anterior glide of the femoral head may be part of a movement impairment syndrome12. I know some trainers and strength coaches are wondering why I have headed down this path, but it is important that we have an understanding of arthrokinematics if we are going to mobilize joints (a.k.a. “mobs” or “joint mobs”). Without research on arthrokinematics, do we really know which way to mobilize a joint? With the introduction of self-administered joint mobilizations into the fitness, strength and conditioning, and clinical realms we must be honest with our current knowledge and supportive of our researchers who may bring clarity and optimization to our interventions. I will make recommendations for hip mobilizations below, although at this point, I could not call my recommendations for hip mobilization evidence-based, only “found to be clinically effective.”

Example of Functional Knee Valgus (Hip Internal Rotation & Adduction)
The Ankle’s Contribution to Knee Dysfunction:
Although, I believe that foot/ankle complex dysfunction and the resultant motion of the tibia plays a large role in knee dysfunction, more evidence is needed. We do have a few references, with a few implications for practice. The most indirect of those references is a study by Frannettovich et al.4, which implies that achilles tendinopathy results in delayed activation of the GMAX and GMED. As discussed above, the inhibition of the GMAX and GMED are also associated with knee dysfunction, potentially implying a link between achilles tendinopathy and future knee issues. A biomechanical link between calcaneal pronation/eversion and hip internal rotation has been noted by Souza et al.7; however, in a study by Powers et al15, the correlation between pronation and knee dysfunction was not found to be as strong as the correlation between knee dysfunction and hip internal rotation7, 15.
The most direct evidence I have found relating foot/ankle complex dysfunction to knee dysfunction is as study by Padua et al10, in which individuals with knee valgus showed not only changes in hip muscle activity, but alterations in activity of invertors, evertors and a correlation between knee valgus and a lack of dorsiflexion. The exciting implications of this study are actually demonstrated in a follow-up study by this group, in which release and lengthening of the adductors, calves and peroneals, along with activation of the invertors of the ankle resulted in reduced knee valgus16.
Although none of these studies are directly correlated with knee pain, they are associated with a pattern of compensation commonly associated with knee dysfunction (hip internal rotation and adduction). I think there is certainly enough evidence to warrant our attention in practice, and my prediction is more research linking the foot/ankle to knee and hip impairment will be published in the near future. At the very least, these studies imply ankle mobility and activation of the invertors may improve lower extremity mechanics, adding a few more tools to our repertoire.

A look at ankle kinematics – http://www.pt.ntu.edu.tw/hmchai/Kinesiology/KINlower/Foot.files/STJclosedKinematics.jpg
A Little Icing on the Cake – The Biceps Femoris:
The biceps femoris has been noted as over-active in those with knee valgus10. It is interesting to note that the short head of the biceps femoris (flexion, external rotation and valgus force) may be the functional antagonist of the VMO (extension, internal rotation?, and varus force). In a study by Hasegawa et al., stretching the biceps femoris actually increased the relative activity of the VMO17. Biceps femoris release and active stretching was included in a study mentioned previously that showed a reduction in knee valgus using selected exercise interventions16.
Pre-hab or Rehab:
As noted above, pain and dysfunction will lead to changes in muscle activity, motor control, joint motion and flexibility. However, many clinicians have considered the possibility that these alterations in the human movement system were not just the result of pain and acute injury, but potentially a cause. We could think of this as a “chick or the egg” scenario. Unfortunately, researching the cause of injury is not as easy as researching individuals who have been injured. Obviously, you cannot impart dysfunction, or intend to injure an individual (that whole ethics thing). Long term studies that observe the multiple factors that could contribute to injury, as well as, record the rate of injury within a population are expensive, so… we have very few. But in the case of knee dysfunction we may be able to link 4 studies that demonstrate our power to reduce the risk of injury.
In a study by Hewet et al.19, a strong correlation was found between knee valgus during squatting and landing tasks, and future ACL injuries in female athletes. In a study by Sigward et al.24, the same knee valgus patterns were correlated with hip internal rotation and adduction, along with greater angle of redirection in both men and women, although women tended toward adopting greater valgus angles. Now, if you remember from the reading above, we have a study that notes the neuromuscular characteristics of individuals who demonstrate knee valgus10, and an additional study that demonstrates an exercise intervention aimed at correcting those neuromuscular alterations reduced knee valgus16. The final step, would be a study correlating the exercise intervention with a reduction in the rate of injury in the same population; currently I am not aware of a published study. Again, this may not be direct evidence of our ability to reduce the risk of injury, future pathology, or increase performance via an exercise intervention aimed at correcting alterations in human movement, but it is certainly a strong case.

How do Robert Griffin III knees look in these images taken his rookie year? Could his run of injuries been prevented? – http://www.acceleratesp.com/wp-content/uploads/2014/04/Robert-Griffin.jpg
Integrated Training Model:
Although many would like to deny its existence, a research study by DiStefano et al20, has shown that an integrated training model that includes intervention to correct compensation patterns, as well as, stability, power and agility training to compliment traditional strength exercises results in better performance than traditional isolated strength training. This is especially true of issues like those in those discussed in this article. In this study, the integrated approach resulted in better scores on a standardized movement assessment (LESS test), reducing knee valgus considerably, while the isolated strength training group showed no change in movement. I know that not everyone is a fan of rolling, stretching, mobilizing, activating, core conditioning, and working on stabilization, but the alternative could be injury and decreased performance, and I do not know a single individual who is a fan of performing poorly or being side-lined by injury.
Now, my stance on corrective exercise is simple. You do not have to spend an entire session doing corrective exercise if you use corrective exercise as your warm-up before every training session. All I am asking anyone to do is bundle their flexibility, core and traditional warm-up time (ex. treadmill), and replace it with a circuit of exercise (10 – 20 minutes) that is aimed at optimizing the way you move. In my opinion, the corrective warm-up (a.k.a. movement prep, integrated warm-up) renders the “general warm-up” obsolete. You have 2 choices before you start training – improve the quality of human movement and optimize mechanics, or spend 10 minutes on a treadmill reinforcing your compensation patterns.
Practical Implications
- Decrease activity of adductors and the TFL
- Decrease activity of calf and evertors
- Decrease activity of the biceps femoris
- Mobilize the hip
- Increase dorsiflexion range of motion
- Increase activity and strength of the GMAX and GMED
- Increase activity and strength of the invertors of the ankle
- Increase neuromuscular control of lower extremity
- Integrate new movement pattern
Sample Program (see videos below):
- *Release TFL, adductors, calf and peroneals
- Self-administered hip mobilization
- Self-administered ankle mobilization
- Stretch Hip Flexors, Adductors and Calf
- **Activate gluteus maximus and gluteus medius
- Activate tibialis posterior
- Reactive activation for lower extremity (neuromuscular control)
- Squat to Row (Integration)
*In as study by Mohr et al, it was found that preceding lengthening techniques with foam rolling resulted in greater increases in mobility, when compared to stretching alone21.
**In a study by Kan et al, it was found that adding abduction to gluteus maximus activation reduced activity of the biceps femoris22. Further, in a study by Selkowitz et al, gluteus medius exercise that included hip extension reduced activity of the TFL23.
It Takes Practice:
Initially this “integrated/corrective warm-up” will take longer than the 10-20 minutes that a normal warm-up would take, but practice will decrease the duration considerably. Please be patient, and give yourself, or your client, a chance to become proficient with the techniques. Further, as you become familiar with your own compensation, or that of your clients, you may be able to reduce the number of techniques to those that specifically target the key issues in your personal variation of this compensation pattern.
Further Reading:
The compensations noted in this article, as well as the findings of the research studies cited, closely resemble my predictive model of lower extremity postural dysfunction, Lower Leg Dysfunction (LLD). For more ideas, techniques, and better understanding of how the lower extremity compensates you may find this article of particular interest. A must read for my fellow Human Movement Science Geeks.
Join BrentBrookbush.com to get instant access to 260+ videos, 190+ articles, and 80+ panel discussions in our fully integrated online platform – register here.
As a thank you to Dean Somerset for his willingness to partner with a like-minded professional I am offering all readers of DeanSomerset.com a discount on membership to BrentBrookbush.com.
1. Go to http://www.brentbrookbush.com
2. Enter coupon codes:
DSDiscountMonthly (9.99/month)
DSDicountYearly (109.00/year)
Videos:
TFL Release:
https://www.youtube.com/watch?v=4aiFou_bPm4
Biceps Femoris Release:
https://www.youtube.com/watch?v=m0Mdaumyw-c
Calf Release:
Hip Mobilization (Self-administered):
Kneeling Hip Flexor Stretch (Lengthening for the TFL):
https://www.youtube.com/watch?v=vQ8NJRCSyb4
Calf Stretch:
Quick Glute Activation Circuit:
Special thanks to my team of writers for reviewing much of the research that is cited in this article:
- Stefanie DiCarrado, DPT, PT, NASM CPT & CES
- Jinny McGivern, DPT, PT, Certified Yoga Instructor
- John Snyder, DPT, PT, CSCS
Bibliography (Note: Many of the studies are linked to reviews of the research study at BrentBrookbush.com)
- Noehren B, Hamill J, Davis I. Prospective Evidence for a Hip Etiology in Patellofemoral Pain. Medicine & Science in Sports & Exercise. 2013;45(6):1120–1124. ABSTRACT
- Qi W. Effect of Increased Iliotibial Band Load on Tibiofemoral Kinematics and Force Distributions: A Direct Measurement in Cadaveric Knees. Journal of Orthopaedic & Sports Physical Therapy. 2013;43(7):478–485.
- Hewett TE, et al. Biomechanical Measures of Neuromuscular Control and Valgus Loading of the Knee Predict Anterior Cruciate Ligament Injury Risk in Female Athletes: A Prospective Study. American Journal of Sports Medicine. 2005;33(4):492–501.
- Franettovich, SM, Honeywill, C, Wyndow N, Crossley KM, Creaby MW. Neuromotor control of gluteal muscles in runners with achilles tendinopathy. Medicine and science in sports and exercise. 2014; 46(3): 594-599.
- Powers CM. The Influence of Abnormal Hip Mechanics on Knee Injury: A Biomechanical Perspective. Journal of Orthopaedic & Sports Physical Therapy. 2010;40(2):42–51. doi:10.2519/jospt.2010.3337.
- Powers CM, Ho K-Y, CHEN Y-J, Souza RB, Farrokhi S. Patellofemoral Joint Stress During Weight-Bearing and Non—Weight-Bearing Quadriceps Exercises. Journal of Orthopaedic & Sports Physical Therapy. 2014;44(5):320–327. doi:10.2519/jospt.2014.4936.
- Willson JD, Davis IS. Lower extremity mechanics of females with and without patellofemoral pain across activities with progressively greater task demands. Clin Biomech. 2008; 23(2): 203-11.
- Noehren B, Scholz J, Davis I. The effect of real-time gait retraining on hip kinematics, pain and function in subjects with patellofemoral pain syndrome. Br J Sports Med. 2011; 45(9): 691-6.
- Nakagawa TH, et al. Frontal Plane Biomechanics in Males and Females with and without Patellofemoral Pain. Medicine & Science in Sports & Exercise. 2012; 44(9): 1747-1755.
- Padua, D. A., Bell, D. R., & Clark, M. A. (2012). Neuromuscular characteristics of individuals displaying excessive medial knee displacement. Journal of athletic training, 47(5), 525.
- Mauntel, T., Begalle, R., Cram, T., Frank, B., Hirth, C., Blackburn, T., & Padua, D. (2013). The effects of lower extremity muscle activation and passive range of motion on single leg squat performance.Journal Of Strength And Conditioning Research / National Strength & Conditioning Association, 27(7), 1813-1823.
- Shirley A Sahrmann, Diagnoses and Treatment of Movement Impairment Syndromes,© 2002 Mosby Inc.
- Grimaldi, A., Richardson, C., Durbridge, G., Donnelly, W., Darnell, R., Hides, J. (2009). The association between degenerative hip joint pathology and size of the gluteus maximus and tensor fascia latae muscles. Manual Therapy. 14. 611-617
- Tateuchi, H., Taniguchi, M., Mori, N., Ichihashi, N. Balance of hip and trunk muscle activity is associated with increased anterior pelvic tilt during prone hip extension (2013) Journal of Electromyography and Kinesiology22 (3). 391-397
- Souza, T. R., Pinto, R. Z., Trede, R. G., Kirkwood, R. N., & Fonseca, S. T. (2010). Temporal couplings between rearfoot–shank complex and hip jointduring walking. Clinical biomechanics, 25(7), 745-748.
- Bell, D. R., Oates, D. C., Clark, M. A., & Padua, D. A. (2013). Two-and 3-dimensional knee valgus are reduced after an exercise intervention in young adults with demonstrable valgus during squatting. Journal of athletic training,48(4), 442-449.
- Hasegawa, K. T., Hori, S., Tsujita, J., & Dawson, M. L. (2001). Effects of Stretching Exercises on Vastus Medialis and Vastus Lateralis.Medicine & Science in Sports & Exercise, 33(5), S10.
- Smith, J. A., Popovich, J. M., & Kulig, K. (2014). The influence of hip strength on lower limb, pelvis, and trunk kinematics and coordination patterns during walking and hopping in healthy women. Journal of Orthopaedic & Sports Physical Therapy, (Early Access), 1-23.
- Hewett, T. E., Myer, G. D., Ford, K. R., Heidt, R. S., Colosimo, A. J., McLean, S. G., & Succop, P. (2005). Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes A prospective study. The American journal of sports medicine, 33(4), 492-501.
- DiStefano, L., DiStefano, M., Frank, B., Clark, M., and Padua, D. (2013). Comparison of integrated and isolated training on performance measures and neuromuscular control. Journal of Strength and Conditioning Research/National Strength & Conditioning Association. 27(4), 1083-1090.
- Mohr, A. R., Long, B. C., & Goad, C. L. (forthcoming 2014). Foam Rolling and Static Stretching on Passive Hip Flexion Range of Motion. Journal of sport rehabilitation. Currently in press.
- Kan, S., Jeon, H., Kwon, O., Cynn, H., Choi, B. (2013). Activation of the gluteus maximus and hamstring muscles during prone hip extension with knee flexion in three hip abduction positions. Manual Therapy18, 303-307
- Selkowitz, D. M., Beneck, G. J., & Powers, C. M. (2013). Which exercises target the gluteal muscles while minimizing activation of the tensor fascia lata? electromyographic assessment using fine-wire electrodes. journal of orthopaedic & sports physical therapy, 43(2), 54-64.
- Sigward S, Cesar G, Havens K. Predictors of Frontal Plane Knee Moments During Side-Step Cutting to 45 and 110 Degrees in Men and Women: Implications for Anterior Cruciate Ligament Injury. Clinical Journal Of Sport Medicine: Official Journal Of The Canadian Academy Of Sport Medicine [serial online]. October 6, 2014;Available from: MEDLINE Complete, Ipswich, MA. Accessed January 29, 2015.
Join BrentBrookbush.com to get instant access to 260+ videos, 190+ articles, and 80+ panel discussions in our fully integrated online platform – register here.
As a thank you to Dean Somerset for his willingness to partner with a like-minded professional I am offering all readers of https://deansomerset.com/ a discount on membership to BrentBrookbush.com. Enter coupon codes:
DSDiscountMonthly (9.99/month)
DSDicountYearly (109.00/year)
© 2015 Brent Brookbush
Questions, comments, and criticisms are welcomed and encouraged –
2 Responses to A More Sophisticated Approach to Correcting Knee Dysfunction