Red Flags You Should Really Be Aware Of
Today’s guest post comes from Dr. Spencer Nadolesky, MD. Spencer and I have connected sporadically through Facebook and Twitter, as well as through email. He’s one of the “new wave” of physicians who is looking at health and active prevention of medical conditions versus the old guard who only treat once an issue has become a problem. He’s also averse to wearing shirts, and according to his pictures on Facebook, training legs.
In all seriousness, I have the utmost respect for Spencer due to his willingness to dispense quality medial and exercise information, help people get fit and healthy, and also have a sense of humour about it all at the same time. Without further adieu, I’ll let him tell you some stuff about back pain you should have on your radar.
Low back pain is not only one of the most common complaints in my family medicine clinic, it is also rampant among fitness enthusiasts on the internet. In Dean’s article, Do You Really Need an MRI?, he mentioned how going to the doctor will help you make sure nothing too serious is causing your lower back pain. But what are those serious causes of pain? In addition, what are the signs and red flags that should cause you to send your client straight to the doc (or yourself if it is you with the pain)? Can you fix all types of back pain with some planks and bird dogs? There are also causes of back pain that have nothing to do with the musculoskeletal system and are not as serious but still best left up to the doctor. Let’s go over two cases.
Kristine was one of my pleasant young female patients at 33 years old. She came to me with her usual low back pain that I was trying to help her with but now she was having some pain that radiated down her leg. After some talking there was some questionable urinary incontinence, although her previous records showed some of the same. Not taking a chance I decided to order the MRI. Unfortunately the insurance company DENIED it and said that there wasn’t enough compelling evidence to warrant the MRI.
A day goes by and the patient calls me telling me that the pain is getting worse and that her “private parts” are now numb. I tried to order the MRI again based on this information and again I was denied. Luckily there is an appeal system so I basically begged the doctor on the other line that was making the decision and we got the MRI that day. The result? A big protrusion of one of lumbar discs causing mass effect in the cauda equina. I immediately got the patient in the hands of the neurosurgeon, who took her to surgery that day.
What were the red flags?
1. Bladder and/or Bowel Incontinence
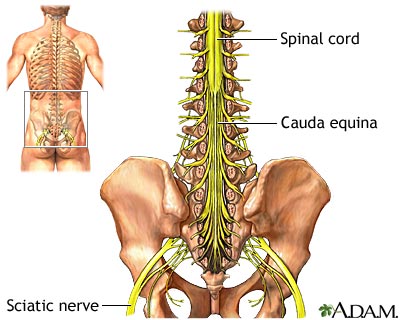
Okay I admit that peeing and/or pooping yourself along with lower back pain may seem like an obvious problem but if it comes it may be subtle like the case above. This is one of those classic medical school board exam questions that no doctor wants to miss. It shouldn’t be one you miss either. This is a sign of possible cauda equina syndrome, which is a medical emergency. The cauda equina is a bundle of nerves located in your lumbar spine, which innervate your lower body including your pelvic organs.
The syndrome can be caused by a tumor, but in the fitness enthusiast population it will likely be a big disc herniation. Either way, this is a medical emergency because the damage can be permanent.
2. Saddle Anesthesia
Another classic sign of cauda equina syndrome you won’t want to miss is saddle anesthesia, where your inner thighs and genital region goes numb. Again, this might seem like an obvious problem, but some folks may not realize this is serious issue. In the case above, I actually had to ask a few questions before she told me that her “private parts” were numb. A physical exam usually goes along with this to check certain reflexes, strength, sensation, and even rectal tone. The bottom line is that if there is even a question of this, the doc should do an exam.
If you remember these red flags, you will hopefully not miss the low back pain cause that is a surgical emergency. There are other serious causes of low back pain but cauda equina syndrome is the one I don’t want you to miss since it needs to be fixed quickly. Remember that back pain can mean a serious underlying issue that needs a doctor to address so be careful!
What about a non-serious cause of back pain that still needs a doctor?
Jennifer was a 21 year old fitness buff. She LOVED lifting weights however every month during her period she was put out of commision for 3 whole days due to low back pain. This is a classic presentation of what is called dymenorrhea. The doctor is generally needed in order to sort out whether this is primary dysmenorrhea or secondary. Secondary dysmenorrhea is pain during a period caused by an identifiable condition such as ovarian cysts or endometriosis, whereas primary has no identifiable cause.
Since Jennifer had no risk factors for other causes such as being over the age 25, pain with sexual intercouse, abnormal amounts of bleeding, and non-midline pain, I diagnosed her with primary dysmenorrhea. To treat her, all I did was put her on a combined estrogen-progestin oral contraceptive (birth control) to take daily along with 400 mg of ibuprofen every 6 hours only during her pain. These methods are by far the best for primary dysmenorrhea, but there is also hope for a combination of B1/B6, fish oil, and vitamin D to help combat this monthly pain (1,2,3,4). Jennifer’s pain went from a 9/10 down to a tolerable 3/10, which she greatly appreciated since she was able to lift during her period from then on.
So you can see, here are two issues that should be handled by the doctor, with one being an emergency and one being just annoying. Either way it is important to know when to refer out to your client’s physician.
Dr. Spencer Nadolsky is an osteopathic family physician who specializes in weight loss (bariatric medicine) and cholesterol (lipidology). While earning a BA in exercise science In undergrad he wrestled heavyweight for the UNC Tar Heels and was ranked as high as 3rd in the nation at one point while also garnering Academic All-American status. You can checkout his blog at www.GetLeanRx.com and his company at www.LeanerLiving.com or connect with him on facebook at https://www.facebook.com/DrSpencerNadolsky and https://www.facebook.com/leanerliving
- Marjoribanks J, Proctor M, Farquhar C, Derks RS. Nonsteroidal anti-inflammatory drugs for dysmenorrhoea. Cochrane Database Syst Rev 2010; :CD001751.
- Wong CL, Farquhar C, Roberts H, Proctor M. Oral contraceptive pill for primary dysmenorrhoea. Cochrane Database Syst Rev 2009; :CD002120.
- Proctor ML, Murphy PA. Herbal and dietary therapies for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev 2001; :CD002124.
- Lasco A, Catalano A, Benvenga S. Improvement of primary dysmenorrhea caused by a single oral dose of vitamin D: results of a randomized, double-blind, placebo-controlled study. Arch Intern Med 2012; 172:366.

7 Responses to Red Flags You Should Really Be Aware Of