Do Leg Length Discrepancies Actually Matter?
Over the years I’ve had a lot of clients with various ailments say they have been diagnosed by different medical practitioners as having a leg length discrepancy, where one leg is longer than the other, and that this difference is a causative or contributing factor to their problems.

Image credit: https://orthoinfo.aaos.org/en/diseases–conditions/limb-length-discrepancy/
In many cases, the leg length isn’t notably different like the pic above. They’re more minor, usually within 10-15 mm, which seems like a pretty small difference to be causing so many issues.
Usually the recommendation to correct this is to use various shoe inserts, from heel pads to insoles, and even custom-made shoes to help relieve some of the difference between the legs.
In today’s post, I wanted to delve into this topic with some specific questions:
- How accurate are the assessments for leg length?
- Is there evidence in the research to show this difference actually causes or contributes to mechanical dysfunction?
- Do shoe inserts actually provide any benefit to treating this condition?
But first, let’s talk about what leg length discrepancies actually are.
True Leg Length Discrepancy: This is where the bones are longer on one side than the other. Some studies have found that up to 90% of the population has a measurable difference in leg length, with 20% showing a difference in length larger than 9mm, or almost half an inch.
Functional Leg Length Discrepancy: This is when the joint on one side don’t line up in the same way as the other, like with a flat foot, valgus collapse on one knee, torsioned pelvis, etc, which causes the impression of a short leg.
Kamis. J Orthop. 2017 Jun; 14(2): 276–280.
How Accurate are Assessments?
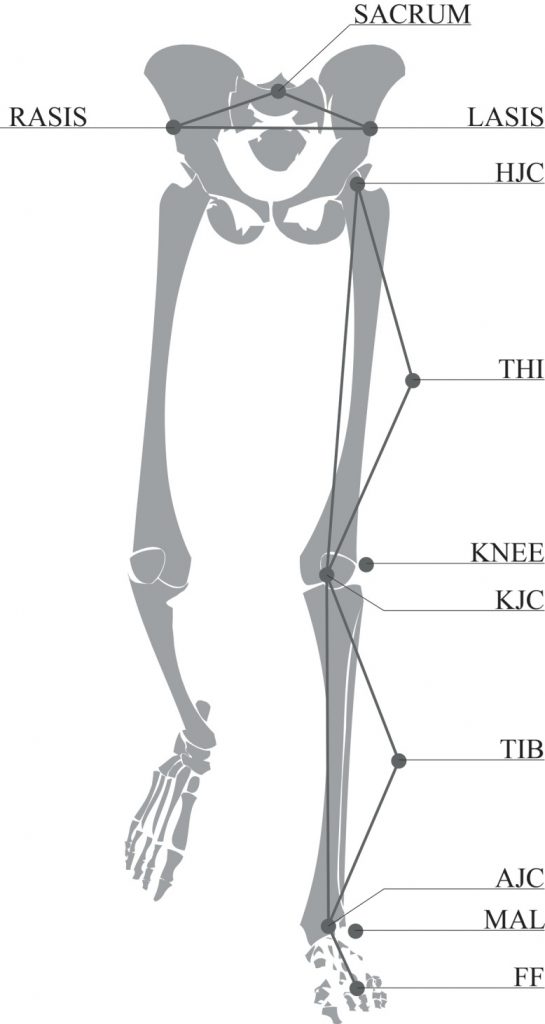
Common approaches to measuring leg length differences are to use wooden blocks to achieve a “neutral” pelvic position, as shown above, as well as tape measurements to measure the length of femurs and tibias on both sides of the body. While these are cost-effective and easy to administer, the accuracy and reliability may be considerably low.
Hanada et al (2001) showed that while tape measurements could be easily reproduced with a high degree of agreement, but only moderate validity compared to radiographic measurements, and only in normal pelvii without gross asymmetry. As I’ve shown previously, you can have a significant difference between left and right hips, within what would be classified as “normal” ranges.
Frieberg et al (Int Disabit Stud. 1988;10(2):49–53) found the error of tape measures was plus/minus 8.4 mm compared to radiologic measurements. They also found the indirect method of using wood blocks to level the pelvis lead to a 53% erroneous measurement rate when leg length differences were greater than 5 mm.
To compound the measurement issues, Gurney showed that clinicians have trouble determining what constitutes a discrepancy requiring intervention, with some citing differences of 5mm or less, and others not worrying until the difference is greater than 20-30mm. With common clinical measurements listed above having relative error rates of 5-10mm, and no specific agreement as to a cut-off point as to when to intervene, it’s tough to say what quantified measured difference is important, especially at lower differences.
Interestingly, few studies compare leg length differences as a factor relative to the individuals’ height, which is strange as a 5 mm difference would be a larger relative difference to someone who is only 5 foot tall compared to someone who is 6’6″.
So to recap:
- Error in clinical measurements can be anywhere from 5-10 mm plus or minus
- no established cut off as to what would be significant enough to warrant intervention
- most measures don’t take into account the individuals height,
Evidence It Contributes To Dysfunction?
The existing body of research has done a rough job at determining if leg length differences are a challenge, how much of a difference is required to affect the individual, what interventions would be most appropriate, and what those interventions success rates actually are.
A metanalysis from Azizan et al showed that while kinematic differences did exist in both gait and balance considerations with increasing leg length differences, there were no discernable differences in those who had symptoms associated with their leg length differences and asymptomatic test subjects, when matched for discrepancy size. The biggest differences came in those with leg length discrepancies following knee and hip replacement surgeries.
Interestingly, the type of approach used for a total hip replacement could affect the size of the post-operative discrepancy, but not very often. Debi et al showed that direct anterior approaches could have a range of discrepancy of -6 to +5mm, lateral approaches had a range of -22 to +14 mm, however the occurrence of a discrepancy greater than 10 mm was only 2.1%
Further in total hip replacement categories, many studies have found that complete reduction of discrepancy realistically can’t happen, even through precise surgical measurements. Some studies have shown there is no correlation to post-operative outcomes and any leg length discrepancies. Others showed that with relatively large differences, patients who were made aware of a leg length difference were less satisfied and required more mobility assistance following their surgery.
in lumbar disc herniation patients (L4-5 and L5S1 predominantly), ten Brinke et al showed pain affecting the short side leg (measured as greater than 1mm. Wait what??) was essentially a coin flip, with 43.8% of men having symptoms into their shorter leg, and 55.9% of women having their shorter leg affected.
Betsch et al simulated difference with various height wood blocks and observed some mild pelvic torsion and repositioning as simulated discrepancies increased, but did not observe any more than minor spinal positional changes with these increasing differences.
So in people going through a total hip replacement, there’s no consensus as to whether a leg length difference is a factor in mobility issues, pain, or other functions, and there’s no clearly defined cut-off as to a difference that would be considered clinically significant.
Even more interesting, comparing trans-femoral amputees with back pain and without back pain, Morgenroth et al found there was no statistical association with limb length and back pain prevalence. Esposito & Russell compared amputees with and without back pain to able-bodied controls, and found pelvic and trunk coordination in amputees with back pain and able-bodied controls with back pain were similar, and the only notable difference between gait patterns of asymptomatic amputees and back pain amputees was in the transverse plane.
So to recap:
- No specific discrepancy shown to affect symptoms, gait mechanics, etc
- no agreement following total hip replacement as to whether leg length discrepancy is impactful on quality of life, or even what the size of that discrepancy would be that could affect quality of life
- no specific difference in back pain prevalence among amputees with various differences in measured and prosthetic-aided leg length discrepancies, and only small differences in gait mechanics in continuous relative phase measurements between asymptomatic amputees and non-pained able-bodied controls
Do Insoles Actually Provide Any Benefit?
The main purpose to using an insole or insert is to minimize the leg length difference, so if it’s an effective treatment for this condition, the research should show that fairly consistently, or at least give some success rates of this application.
There are a number of studies that show use of inserts are very beneficial, however it should be noted these studies showed the greatest outcomes at differences of 10 mm or less, and as mentioned earlier, most clinical assessments have an error rate of 5-10 mm, and many researchers caution against providing treatments for differences of under 10 mm, or less than 1/2 inch.
In distance runners, Gross et al showed inserts were beneficial for reducing or greatly improving symptoms associated with running, of which leg length discrepancy was a factor in the subjects self-reported responses of injuries (13.5% of conditions reported).
A systematic review of all literature by Campbell et al showed there was low quality evidence, but evidence nonetheless, that orthotics could positively affect low back pain. However the author noted that many of the studies with a very broad effect size through studies.
So to recap:
- inserts used for less than 10 mm discrepancies seem beneficial, but errors in measurement may reduce this benefit to simple placebo.
- Runners with a higher impact and mileage, who are symptomatic for various lower leg issues, can benefit from inserts, but much of the data for other participants needs to be carried out with higher quality studies.
- There’s no agreement as to whether inserts relieve symptoms based on the breadth of the available research
Overview
In general, there doesn’t seem to be much of a consensus on the role of a leg length issue in injuries, tissue tolerances, stressors through the knees, hips or low back. There’s also significant measurement issues, especially for any diagnosis of discrepancies of less than 10 mm.
Amputees, who could be said to have the most extreme case of leg length discrepancies, don’t show consistency when it comes to symptoms relative to the length and fit of prosthesis, and when compared to able-bodied controls, symptomatic and asymptomatic amputees don’t seem to present differently relative to their impacted leg length discrepancy.
Inserts don’t seem to have definitive success rate when it comes to relieving symptoms believed to be related to leg length discrepancies, other than a possible placebo effect.
Recommendations
So what do you do if you have a leg length discrepancy that you feel is causing you issues? There’s a few options you could go through for conservative treatments and training.
- Physio or manual therapy to help with any overworked tissues, retrain joint alignment as much as possible, and improve balance. These seem have big effects on managing symptoms with as much success as anything.
- Try inserts if you have a medical plan that will pay for them. If not, they can be a few hundred bucks, so weigh the pro with the cons on that one. Just note that semi-solid or soft inserts will wear out within a couple years, so you’ll have to buy new ones down the road if you do notice a benefit. If you don’t feel a significant benefit within a few weeks, it’s probably not benefitting you much at all. Before you shell out though, go to a drug store and get a cheap set of Dr. Scholls inserts and see if they make any tangible difference. They go for only a couple of dollars.
- Do more unilateral leg training to avoid getting stuck in a bilateral stance, especially under loading. Alternatively, if you want to do bilateral stuff like squats or deadlifts, play with your stance to see if an asymmetric stance makes you feel more stable and strong.split squats, single leg deadlifts, and lunges are all awesome variations that should be in your program already.
- Walk on varied surfaces as much as possible. We have a huge variability in our bodies and we can adapt to a lot of stuff, so putting your body in a position where it doesn’t have to conform to a constantly flat and level footing can go a long way to avoiding potential movement pattern overload, which may contribute to symptoms associated with leg length issues.
- Train in a variety of movements, directions, and loading scenarios. Variety helps break up monotony, and bodies seem to enjoy a little spice on occasion.
One thing that’s also worth noting is that it’s really difficult to connect the dots between a potential biomechanical feature and pain. Pain is a multifactorial concept, and often biomechanics are simply a small part of that. The body is great at compensating to find the least energetically expensive and least painful way of doing things, so if that means the longer leg winds up with a flatter arch, a rotated knee, or slightly asymmetrical stance, it will find a way. This isn’t to say that there isn’t a connection with biomechanics, but that only chasing a treatment of reducing the potential discrepancy likely won’t fix all of the problems that may be contributing to pain, symptoms, or side effects of treatment.