Checklist for Determining Movement Dysfunctions and How to Get Over Them
I’ve been working with people for the better part of the last decade, trying to get them to move without as much resistance to unloaded movements, get through sticky tissues (either from scar tissue from surgery, dehydration, or anything else that can make you “stiff”), work within their capabilities, and then get after it to become the most jacked dieseled out beast of a human being possible. This means getting people with a knee replacement to progress up through strength and conditioning to do sled sprints, getting rotator cuff repair clients to own kettlebell swings and farmer carries, and pelvic floor surgical reconstruction clients to deadlift twice their body weight.
This is not me blowing my own horn as a trainer. Honestly, there’s a lot of other folks out there who can do this and probably do it better. There’s people who understand injuries a lot more than I do, and I will never match a physiotherapist in terms of treatment because I’ve never received the formal training they have.
That said, I’m pretty good at some of the things I normally do.
[embedplusvideo height=”367″ width=”600″ editlink=”http://bit.ly/1pTO6mR” standard=”http://www.youtube.com/v/2fzDw-vgQZ4?fs=1″ vars=”ytid=2fzDw-vgQZ4&width=600&height=367&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep5562″ /]
Assessments are a time to ask questions, not to take measurements.
If someone comes into me for training and they say they want to get stronger, but have no issues with previous injuries, trauma, or whatever, I could screen them and come up with all types of numbers, then design corrective strategies as to how to fix problems they weren’t aware of, but in most instances, those won’t translate well into getting stronger unless we address a couple of key components behind them.
For instance, let’s say we assess someone’s ability to squat, and it winds up looking like a rusty hinge. the person is in their early thirties, with no history of trauma, so degenerative changes and osteoarthritis shouldn’t be a limiting factor, so what gives? Should we load it up and see whether more weight helps clear it up? That’s an option that typically (about 99% of the time, anyway) produces terrible adaptations.
Now let’s say we screen them and then set up in a corrective sequence based on what we think is going on, spend 10 weeks working on it, then re-test and see……… the exact same squat pattern. did the person get stronger? Absolutely. If you give them stressors that they have to adapt to, they’re going to adapt and get stronger. However, if the issue being corrected wasn’t the main affect against the individual doing a squat pattern, it won’t help. It’s time to move on and refund the last 10 weeks of training fees.
Simply put, corrective exercises should correct something. The aspect that should be corrected should be something that gets measurable improvements in a relatively short period of time. The girl doing the side plank int he video above? She saw improvements in a couple of minutes to visibly see changes in her range of motion. It was an applicable strategy for her, and the re-test showed improvements.
Now let’s say you get someone who doesn’t respond to the side plank the way the girl in the video did. What gives? Is the exercise broken? Are you doing it wrong? Maybe, but most likely, it’s not the right approach for that individual, and the reason they’re seeing some form of restriction is probably found elsewhere.
Today I wanted to break down a simple check list I use to determine the causative factors behind any movement restriction, and then show some ways to make them better.
#1: Structural Restrictions
We always assume everyone has the same bones and joints, muscles and attachment points, and lever lengths when it comes to exercise. We know this isn’t true, but it doesn’t stop us all from making the same assumptions. If it were the case, we wouldn’t have centres in basketball, and the Mountain would only be 5’10” and 200 lbs, not a 6’9″ 420 pound monster from Iceland.
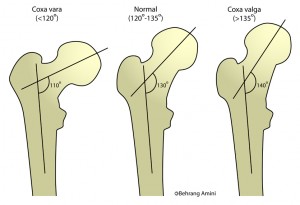
The femur as it inserts into the hip joint can have a couple of different variations. The first is in the vertical angle of the femoral neck. The three major positions can provide a massive variation from one end of the spectrum to the other. The second aspect is the anterior-posterior variation of the femur. The third aspect to look at is the positioning of the acetabulum and whether it sits more anterior, posterior, or vertical. There’s 27 potential combinations of femur and acetabular alignments, which means there’s potentially 27 different “optimal” positions for people to find their best squat pattern, or that could resist performing a squat.
When two bones get close to each other, they compress any kind of tissues that can be in between them. Try this out: Make two fists and press them together as far as possible. You’re only going to be able to press into contact so far before either physically you can’t do it any more or pain prevents further movement from happening. If you want to go further, you’re going to damage something. For the squat, the bones of the femoral neck and the ridge of the acetabulum come closer together, and eventually, they can’t get any further without creating bone to bone contact, and further movement in that position will either cause pain or other problems.
One option that could present with the hips is femoral acetabular impingement, where a bony outgrowth is created on either the femoral neck (cam) or the acetabular ridge (pincher) that creates earlier bone to bone contact, therefore restricting mobility.
One way to look at this is with a simple Thomas test. Grab your knee, roll onto your back and hug your knee as tight to your chest as you can. If the other leg dangles and your hips haven’t rolled back so your tailbone is off the ground, and if it’s not painful, you have enough range of motion to do a squat from a structural perspective.
[embedplusvideo height=”479″ width=”600″ editlink=”http://bit.ly/1pTT4QL” standard=”http://www.youtube.com/v/5_IpvJJcH5U?fs=1″ vars=”ytid=5_IpvJJcH5U&width=600&height=479&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep8302″ /]
The ankle is very similar. If you were to go into the operating room and get a dose of anaesthesia from a qualified health professional (not some back alley salesman with a gold tooth and a shifty glare), your ankle will most likely flop around like a dead fish. If you have a history of ankle injuries or some form of degenerative change, your ankle will be pretty stiff. I’ve rolled my right ankle more times than I can count (I run out of fingers after 10 and then counting gets dodgy), so my mobility, specifically through dorsiflexion and internal rotation is minimal.
[embedplusvideo height=”367″ width=”600″ editlink=”http://bit.ly/1pTSAKi” standard=”http://www.youtube.com/v/ce690C-Hjio?fs=1″ vars=”ytid=ce690C-Hjio&width=600&height=367&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep7592″ /]
This is a very short outline of some of the structural issues that could present with a squat pattern. The end result of all this is to say, is there something anatomically that’s holding you back, or that you need to adjust?
From a structural perspective, if they have more than enough range of motion through passive means like these, the realistic conclusion could be that they have the structural ability to get through the movement. If these passive movements are restricted, they could have structural issues, or potentially soft tissue issues, guarding tension, or other problems keeping them from doing the movement.
Essentially,
Passive mobility is the available range of motion that you could theoretically use actively.
If you can get your knee to your chest and dorsiflex your ankle, all while having your hamstrings touch your calves, that’s a squat range of motion. Another way to view this is through a simple rock back with the ankles in dorsiflexion. This is essentially a horizontal squat. If they can do that, the structure and soft tissue aren’t restricted enough to prevent the squat from happening vertically.
[embedplusvideo height=”479″ width=”600″ editlink=”http://bit.ly/1hfA679″ standard=”http://www.youtube.com/v/Gzj9AOn4KDY?fs=1″ vars=”ytid=Gzj9AOn4KDY&width=600&height=479&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep8653″ /]
Now if this issue is related to structural alterations or possible degeneration or dysfunction, you’re stuck between a literal rock and a hard place. You can’t stretch out bone to bone contact. You can’t foam roll joint space narrowing. You can’t use manual therapy or acupuncture to release arthritis. You can use all of those modalities for other things, but if the structure is the limiting factor, the only thing that will fix that is surgery to alter the bone shape and alignment. That’s what happens with joint replacements. The only way someone with severe osteoarthritis will regain their range of motion in their locked up knee will be to get a bionic new one made of titanium and kevlar, maybe even some adamantium with optional sunroofs.
If someone can’t get to a full depth squat due to structural limitations, that’s fine. We can use what they have available to use as best as possible. Box squats, assisted squats, and working towards their tolerance is still applicable, but they won’t be able to get to what would be considered “optimal” because their joints don’t let them get there.
Occasionally this can be adjusted by simply altering the set up, or the foot positioning. Some people get much better results from taking a wider stance, some by turning their toes out, and some others by simply altering whether they press through their heels or toes. For me, I can usually have better depth with a wider toe out positioning, but I can still do it with my heels relatively close. When my knees come in, my heels have to go out a little wider.
[embedplusvideo height=”367″ width=”600″ editlink=”http://bit.ly/1hfFWFH” standard=”http://www.youtube.com/v/XVMjwzGotKc?fs=1″ vars=”ytid=XVMjwzGotKc&width=600&height=367&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep3333″ /]
[embedplusvideo height=”367″ width=”600″ editlink=”http://bit.ly/1hfG5sG” standard=”http://www.youtube.com/v/-TssoTtSi2U?fs=1″ vars=”ytid=-TssoTtSi2U&width=600&height=367&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep7764″ /]
Changing position just changes how the bones come together, giving some additional range of motion or limiting it further, so playing with positioning you can see some significant alterations in whether you can hit depth or not. If you play with positioning and suddenly find a new range of motion, cool. That’s your new position. Use it, and get after it. If changing positioning doesn’t alter your ability to squat, and you have restricted passive mobility, it could be a structural issue. It could be a soft tissue issue. It could be a guarding issue. Right now, we just know it’s restricted. Let’s look further.
#2: Soft Tissue Restrictions
Foam rolling has been shown to help improve range of motion in both clinical and research settings when applied appropriately. I’ve had people do a standing toe touch, get to their knees, roll out their feet and re-test the toe touch and all of a sudden hit the floor with both palms. Similarly, I’ve had clients who couldn’t squat roll out their adductors, swear bloody hell and make some interesting faces, then squat to the floor without restriction. The re-test validates the application.
Soft tissue work through foam rolling or other self-myofascial release, manual therapy like ART, or massage, as well as tool-assisted mechanisms like Graston, acupuncture, or other forms of medieval torture can provide some significant increases in available range of motion, most likely through an alteration in resting neural tone and decreasing guarding tension through the region. If the body is saying “HANG ON!!!” that tissue will stay tight. Moving into tight muscles and other tissues will present some restriction, and it will take some effort to push through, much like trying to push water up hill.
This tension is a good thing when lifting heavier loads, as it prevents you from dropping through to the bottom of your movement and decreasing your power output, as well as preventing you from getting into an end-range of motion where you may not be used to existing, and therefor reducing your likelihood of getting pain from some sort of injury. It’s a necessary adaptation, but typically means you have some weakness at the end range of motion, and that you’re trying to not get there.
Reducing the neural tension driving the muscles to be tight is a good idea before you train a range of motion, but it should be used when you’re looking to train a range of motion, not when you’re just simply going back to work. I’ve worked with a couple of really skilled manual therapists and scheduled training sessions immediately following their treatments, so as soon as they have that new range of motion we could get them into the gym and train their new mobility, while also reinforcing stabilization through the system. It seems to work well.
So if you’re looking to use soft tissue alterations in your assessment, here’s what you do. Check passive range of motion. Check their movement quality and depth. Do soft tissue work, either through manual therapy if you’re a manual therapist or through foam rolling on some areas like the adductors, glutes, IT bands, and calves, then re-test both passive and active patterns. If you see a remarkable difference, cool. The person needs to do soft tissue work before each workout. Odds are 3-8 minutes of rolling on those key areas will show some significant improvements, so make sure you’re keeping a couple minutes of rolling in their warm ups. If they don;t see a difference, cool. That just means we need to look elsewhere.
[embedplusvideo height=”367″ width=”600″ editlink=”http://bit.ly/1hfMeFe” standard=”http://www.youtube.com/v/aU5GYyC6PFw?fs=1″ vars=”ytid=aU5GYyC6PFw&width=600&height=367&start=&stop=&rs=w&hd=0&autoplay=0&react=1&chapters=¬es=” id=”ep4869″ /]
To conclude today’s post, we’ve looked at some of the passive things that can hold back an awesome squat pattern, like the anatomical structural variances and the soft tissue tension that could be guarding against movement. If you can adjust positioning and do some rolling, you can clear up a lot of the passive restrictions that could impede a deep squat, but only to the available range of motion that the person has in their employ. These are more of the “hardware” kinds of restrictions that could occur. Not all, but it accomplishes a lot of the end goals in main components.
The next post will look at some of the motor pattern, dynamic stabilization, and somewhat “software” issues that could arrise to prevent a deep squat from happening and what to do with them.



6 Responses to Checklist for Determining Movement Dysfunctions and How to Get Over Them