Case Study Breakdown
I typically get a lot of people emailing or messaging me trying to figure out some sort of pain or problem they’re having, which is somewhat unfortunate as I’m not really in a position to be able to help them out with a quick “do this and your problems are solved.” I wish it could be that easy, but in many cases the messages I get are something like “Hi Dean, my SI joint hurts, what should I do?” My default answer is “go to see a physical therapist or a doctor,” as the info they give me is very inadequate to make any recommendations, and also I’m not a medical professional and can’t actually make a diagnosis, over the internet or otherwise.
With the previous caveats in place, I wanted to share a potential case study that was emailed to me, not to provide a diagnosis of any kind (again, I can’t) but to simply walk through my process of analysis of the problem and provide a few potential avenues the individual could follow to see if they could get some relief or success. I can’t overstate enough how any of what I am going to say is definitive, or should take the place of a medical diagnosis or personal treatment from a medical professional, but is merely the opinion of some guy on the internet based on the information available at the time. Most of my recommendations will still follow the “go see a doc or physical therapist” route, but this will provide some of the background thinking into why those recommendations are in place. Sound cool? We all on the same page? Great.
So here’s an outline from the source who sent the email, who will remain anonymous:
“1. I have an anterior pelvic tilt and slight kyphotic posture. Rectus femoris seems short by Thomas test.
2. I am unable to sit tall on the ground, legs straight out in front of me. My back goes into posterior pelvic tilt, I feel it in my hamstrings and low back (tightness) but most of all I feel very tight muscles in front of the hip, seems like they are working so hard to keep me in this position. I get tired and unable to hold tall position very fast.
3. I feel hip pain with any movement that you have to spread the legs. For example, adductor stretches (especially when you change sides, very sharp pain), wide stance squat without any weight is painful (and my back goes into crazy anterior pelvic tilt while doing this, pelvic goes to the back, and unable to hold tall/neutral position), simple side leg lifts while standing may feel painful. I can’t spread legs very much even when lying on floor with legs on the wall, very limited range.
4. Sitting on floor with legs straight and open (V sit) is almost impossible. I lean backwards a lot. Same as number 2.
5. Normal squat feels good even with my body weight, deadlifts are OK too. Muscles that are always tight, or I just feel that they are tight, is hamstrings (very limited mobility, very tight), adductors, rectus femoris or quads, and low back. But stretching not seems to help me, I feel that something around my pelvis/hip is too weak or too tight, that in movements I described above, my hip goes out of alignment and sharp pain occurs.”
Form this description, we have pain with abduction of any kind, active or passive, and in either flexion or neutral, as well as limited hip flexion with straight legs. Where the pain is wasn’t disclosed, and could be anterior/groin, adductor attachment, or lateral hip. A restricted Thomas test would give an idea of passive hip flexion capability, which seems reduced (can’t confirm visually from the text), and squats and deadlifts at a flexed hip angle don’t seem to impact unless in a wider stance. There’s a loss of femoropelvic motion during any wide stance work, which could indicate a lack of range of motion in the joint. There’s not a lot of specific info in there to work from other than what I just outlined, so most of the following is going to be more questions and speculation than anything.
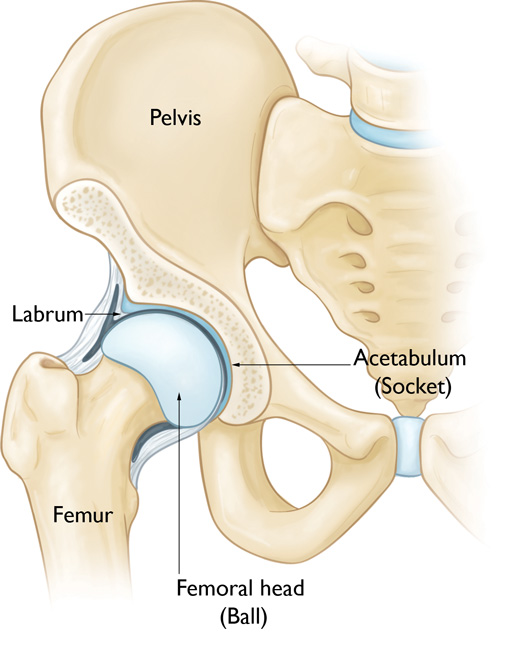
So to begin with, I would want to ask this individual if this is a recent thing they’ve been dealing with, or has this level of hip mobility and pain been a consistent thing for the majority of their life? If someone has always been “tight” and unable to produce a specific range of motion, there’s the potential their structure could be a culprit, which means the shape and angle of their hips would prevent some of the ranges of motion we’re dealing with, but if they were previously very mobile and recently developed issues, the odds of their anatomy changing that quickly is pretty slim without some catastrophic injury. I would think as the abduction movements seem to be painful, they may have a larger center edge angle bilaterally, or potentially some labral tears or other impingement type issues present.
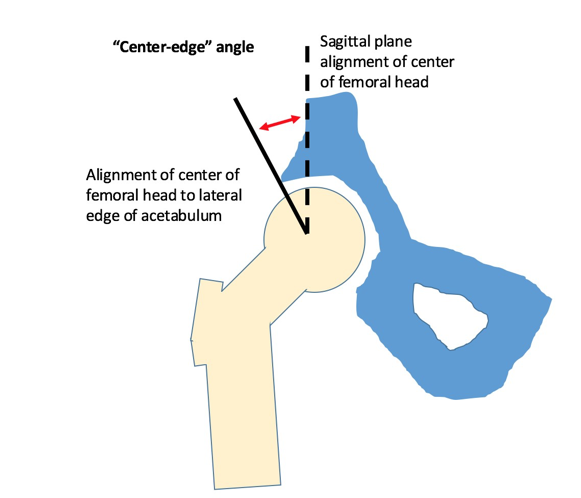
They may also have a retroverted acetabulum, which would make hip flexion positions or movements challenging, as the cup of the hip socket is pointed more posteriorly than anteriorly, which would limit flexion. Some studies have shown positive correlation between pelvic incidence (angle of lumbar spine relative to the femoral neck) and incidence of retroversion, which means it’s a potential predisposing consideration for anyone who has a consistent anterior pelvic tilt. This could be why sitting in a tall kneeling position (pushed more posterior tilt) causes the hip flexors and anterior muscles to feel like they’re working harder as they’re more stretched than usual and under load. When sitting in a tall spine position and legs out in front (deep flexion) the same muscles are working hard to pull into more flexion than the hip may have available.
The only way to truly tell if this is the case is with an X-ray series looking at anterior-posterior as well as lateral views, however you can do a lot in a manual assessment, and potentially a self assessment as well to get an idea of this applies. At this point in the breakdown, it’s speculative if hip anatomy may be a culprit to the issues discussed, and it has some saliency based on pattern of symptoms and correlations to anatomy.
What’s most concerning here is that any abducted position produces pain, whether in a wide stance squat, adductor stretch, or even side lying leg raise. This could be a lateral FAI, potential labral tear, or maybe just a mild greater trochanteric bursitis or adductor tendinitis, but would need further testing to determine. It could also be some mild glute med tendinitis, or IT band friction, but again, it would need further testing to see what’s happening and drill down on the specific etiology of the condition. If normal movement of the hip caused any snapping or catching sensations, it could be more likely linked to a capsular or labral tear than bursitis or tendinitis.
Another question I would ask is whether rotation is affected at all. Internal and external rotation in neutral and in flexion could give some information on whether there’s potential impingement or involvement of capsular or labral issues, as well as the overall shape and orientation of the hip joint. 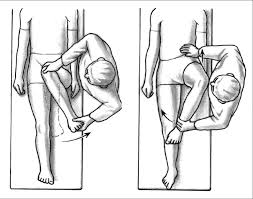
If these movements aren’t affected, fantastic. If they are, we could apply a corrective option like a side plank or even forced breathing to see if it affects the movement, and if it manages to improve it, that’s great too. If retesting some of the previously painful movements improves after this plank and breathing option, we might have some ideas as to what is happening (positional issues that may have been altered from the core stuff, maybe upregulating activity of muscles that weren’t doing something before and are now contributing, etc). If this doesn’t improve passive, and if there’s pain with any of the movements, that’s a red flag. Another red flag is if they can’t achieve a relatively similar rotational position on their own actively.
If flexed and abducted rotations weren’t painful, but strict abductions were, we’d be in a referral situation to see what was happening. Maybe some direct soft tissue work would be all that was needed to reduce the pain and make it workable. Maybe they would need surgery to fix a labral tear with potential FAI bony blocks. If all rotations or even some were painful, they’re still in a referral situation for the same reasons, but now it’s more serious as more movements are negatively affected.
In terms of hip flexion work, if non-painful and improvements in range of motion were actually possible, one way to look at that would be with an FRC corrective option of PAILs and RAILs, or isometric contractions of the hip flexors and extensors in an end-range hip flexion position.
If deep hip flexion improved and wasn’t producing pain, it’s an indicator that limitations aren’t actually structural per se, but could be neural inhibition of some type. Continued work on these as long as pain free and producing results would be indicated. If no improvement was noted following doing these, structure is still on the table as a potential causative factor, but may not be confirmed without other testing or imaging.
Another question I would have at this point would be “what movements do you do really well and that don’t hurt?” If he said a normal stance squat and deadlift were money to him, I’d ask to see what they looked like. If he could hit a deep hip flexion angle with these movements without problems, but couldn’t with any of the other tests, it would show deep hip flexion was possible (likely not structural then), but that his ability to do it in other situations wasn’t there. Maybe it was active control, maybe it was position specific, or maybe he hadn’t developed the motor pattern to get his brain to use that range of motion in other ways. Either way, if I can see a range of motion CAN be achieved somewhere, it’s not structural. If it’s consistently NOT achievable and correctives produce no benefit, structure is a potential limiter.
In terms of the movements that always hurt, maybe there’s a way of adjusting technique or positioning to make them not hurt or at least not hurt as much. If it’s truly a biomechanic issue, maybe it’s something where adjusting the mechanics can adjust the outcome. That would also give information as to whether it’s the TFL, glute med, IT band, etc are working harder and getting some trigger point activation from those movements, which would mean soft tissue work to get through and some movement pattern retraining to help reduce the reliance on those areas to do everything.
If positional alteration didn’t relieve the pain, again it’s a referral. If soft tissue work with a roller or lacrosse ball didn’t work, again it’s a referral. Cough due to cold, it’s a referral. Hang nail = referral. Doubled vision, you like Pepsi over Coke, think Army of Darkness wasn’t that good of a movie, etc etc etc = referral.
By this point in an assessment, I’d have a good idea of whether certain movements were always painful and limited, are so but only in certain situations (positions, angles, level of loading, or whether passive or active), and what ones are not impacted. If some of those previously painful movements or areas can become painless or reduced pain with a simple movement or adjustment to positioning, and also whether something simple like a side plank or breathing has an affect on anything at all. If they can do 3 or 4 things without any problem, but there’s one thing they really want to do that always hurts, or if there’s the odd thing that hurts if they’re not paying attention, and also if there’s any build up that’s lead to this, I’m probably also going to note and make recommendations based on those.
If there’s an inconsistent pattern of things that are problematic, like pain-free passive but painful active, or restricted flexion in this situation but unrestricted in others, that’s something we could likely work with in a gradually progressive manner, but I would still want to have a second set of eyes on the problem. If there was a consistent pattern of pain or discomfort with all elements involving certain movements or characteristics, I’d still want that second set of eyes to see what was going on, and definitely before we started any kind of training.
Where I WOULD say we could begin doing some kind of training is if simple fixes caused a big reduction in symptoms, and those symptoms didn’t return or get worse after the assessment. If range of motion improved immediately with basic correctives, if the stuff that hurt was a benign movement they rarely did and just needed to learn how to control, or if it was a technique issue on a common movement that showed some signficant benefit from technical adjustment and coaching. If these situations weren’t met, they would be referred.
While I know this post doesn’t give any specific information on “if this, you should do that,” that wasn’t the point. I wanted to show how the process of investigation that I use would work, and give some context on how much thought goes into an assessment, how much information is required to make an informed decision, and how many things can go wrong in the process that would make someone a candidate for medical intervention. If it was simple, it would be easy and everyone would do it.
This doesn’t mean to be blind or to not be willing to investigate. It just shows that you have to know what your limits are as a professional, tag out when outside of your scope of practice, and have a network of like-minded professionals who are willing to work with you to find solutions for your clients and their patients. No one wins if you jump the gun and just go for it recklessly, especially if it’s something where a simple fix could be a solution, or where the risks are very real to further damage.
So to answer the emailer in this instance, my professional opinion would be that I can’t help you at this point in time. I would need to see you in person to form an idea of what was going on and whether I would need to refer you to someone for a specific reason or whether it was a simple fix that an exercise or stretch could help. Without this information, it’s almost impossible for me to offer any advice that could be helpful to your specific situation, and would likely either be useless or potentially harmful.
I think that last paragraph will become my boilerplate copy-and-paste statement for future emails or messages.
Let me know what you think of the thought process I used here, if you would do something different, or if you think I missed anything with a comment below.
2 Responses to Case Study Breakdown