Some Big Reasons Why Your IT Band Hurts
I don’t think there’s a day that goes by where someone doesn’t complain about either a knee problem, hip problem, or direct pain associated with the IT band. A lot of the time, lateral knee pain right below the joint tends to correlate really highly to tight IT bands, and when hit up with some SMR and maybe some tac and stretch kind of stuff, although really really, ridiculously painful, it tends to end the knee pain once the person can regain consciousness and not hate life.
The funny thing is, this isn’t just isolated to knee pain. I’ve had some pretty good results at having clients reduce hip and low back tension by getting grimy on their IT band. Why? Well, it’s kind of a big deal part of the body.
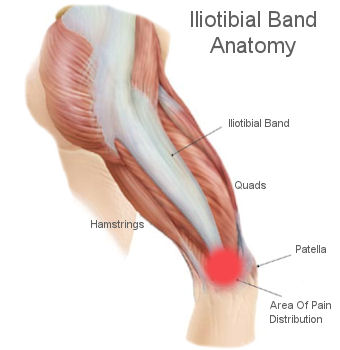
Essentially, the IT band is a thick, thick band of fascia that runs between the glute max & tensor fascia lata and down to the upper lateral part of the tibia.
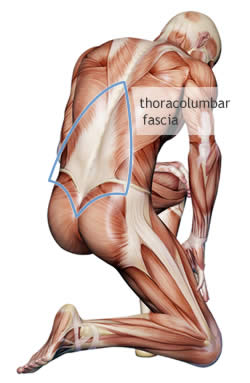
The glute max particularly has some thick and dense connectivity to the IT band with its lateral fibers. Following the chain up, the fascia that connects through the glutes also crosses the SI joint and low back, making this line of tissue incredibly important for the overall function of the hip and low back. When pulled tight, this complex band of tissue can cause the spine, hip and knee to lose its natural alignment, and possibly cause some pain or problems with strength movements. The upper medial fibers also blend into the fibers of the thoracolumbar fascia, which means it has a role in low back structure too.
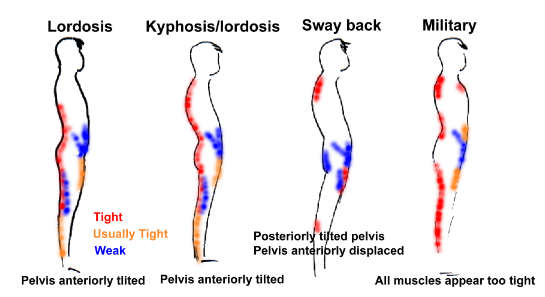
This becomes especially true in individuals who exhibit a more flexion biased posture through their lumbar spine, coupled with a posterior tilted pelvis (think tucking your tailbone between your legs), and a tendency to not straighten the knees completely.
Runners tend to get a lot of IT band issues due to the improper mechanical alignment of stride following fatigue. Most runners tend to run until they can’t tolerate breathing any more before they have to take a rest day, and then are back at it again, shuffling as fast as the pain will allow. I’m not just picking on runners who don’t listen to their bodies: a recent study by Jelsling et al from the Mayo Clinic showed that 100% of the sample of asymptomatic runners had fluid accumulation in their IT bands, which would indicate some sort of inflammatory or high stress state. In 90% of their subjects the fluid was bilateral too.
Another study by Finnof et al looked at injury patterns involving patellofemoral pain among high school runners, and found a greater discrepancy between the hip abductors and adductors (with the abductors being significantly stronger) in the injured population when comparing pre-injury to post-injury strength. The glute max and tensor fascia lata are both abductors, which stands to reason that if they’re working extremely hard, they would generate more tension through the IT band, which operates sort of like a tendon for the two.
I wrote a piece on knee pain and IT bands a couple years ago HERE, so check it out for some additional info if you’re up to it.
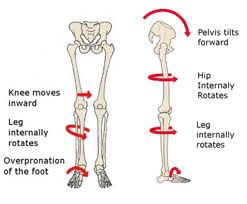
Runners get their IT bands beat up because of the common feature of pronation following fatigue. This pronation causes tibial internal rotation, femoral adduction and internal rotation, and a stretching of the hip abductors, which increases the length and tension applied to the IT band and makes it stupidly unhappy.
The IT band then fights to try to maintain the knee alignment and position during this onslaught, and eventually yeilds to high volume on pavement.
Essentially, the way I view it is that the IT band acts sort of like the E-brake on the knee and hip complex, decelerating rotation that would come from a faulty foot strike or insufficient strength through the hip stabilizers. Since the knee is designed as a hinge joint with very little room for lateral or rotational movement, and the majority of force producing structures are operating through the saggital plane (quads and hammies), the IT band and adductors operate synergistically to help provide some stability against these movements.
In low back pain, there’s a possible link to tightness through the IT band and possible compensatory actions. Arab & Nourbakhsh found there wasn’t a positive correlation between subjects with low back pain and IT band tightness compared to those without IT band tightness, but did show those without low back pain did have significantly stronger abduction strength. Looking at the earlier study about patellofemoral pain and abductor strength, you can see the correlation is possible for the low back too. The study didn’t look at whether relieving the IT band pain through manual therapy would have reduced the low back pain, but it has the possibility to do so.
A commonality of people with low back pain, specifically those in a flexion dominant posture, is reduced glute activity and strength, as well as global hip weakness. These muscles typically are held short and wind up not producing power or contractive capability in favour of using the hamstrings and low back.
The second from right is the typical posture I would see in most middle aged desk jockeys who have a history of non-specific low back pain.
When we begin to get glute activation through modes like hip hinging, bird dogs, squats, and other hip driven movements where the goal is to resist getting the low back to dominate the movement, the glutes wind up getting stronger very quickly.
The downside to strengthening the glutes rapidly is that muscles have the ability to adapt to stressors very quickly, whereas other tissues, such as ligaments and tendons (which the IT band closely resembles on dissection), the adaptive phase takes much longer. Muscles have specialized satellite cells that constantly repair and regenerate muscle tissue damaged from exercise and misuse, which is why you can recover from a tough workout in three days, and why most repetitive strain issues are to attachment tissues such as fascia, tendons and ligaments. Muscles are typically good to go after a couple days and a soak in epsom salts, whereas chronically stressed attachment tissue could take a few weeks to hit the same level of adaptation.
This is one reason why de-load weeks are such a good idea to include in most programs. You may feel absolutely fantastic, but it gives a lower stress time period to allow some catch-up for the attachment tissue to adapt to the level of the muscle without causing a perfect storm of fail that results in your knee feeling achy.
To summarize that last point, if you’re doing a lot of glute work, specifically as a cogent to low back pain or knee pain, you’re indirectly working your IT band, which may not catch up as quickly and could need some serious dedicated soft tissue work, recovery modalities, and de-loads to allow it to not hurt like crazy. Making sweet sweet love to the foam roller should be a daily priority to help reset some of the neural tension through the area, reduce contractile thresholds, and make the area actually move without shifting the joint out of alignment. For more intensive work, try getting some ART or Graston work done, which feels sort of like you’re being gently filleted alive.
The heavier and more specific you’re training your hip extenders, the more you will have to spend time on IT band work to balance the training out and make sure that everything is moving along at the same speed, or roughly the same speed.
IT band issues aren’t typically a big deal unless they’re left to ferment and fester without some quality soft tissue work for an extended time. They usually result in some tenderness, reduced ability to flex the knee without pain, or some form of aching on the lateral thigh, coupled with trigger points around the hip or lower thigh along the lateral line which would make you jump about 6 feet into the air when they’re beat on for a minute. Once given a chance to recover, hit with a roller, and reposition your foot (if you’re a pronator), they usually go away, at least until they get over-stressed again. Then it’s just a matter of diligent work on the area. Consider it sort of like the oil change every 5000km to make sure your car runs smoothly. Hit the roller to start the workout, as needed after the workout, and IT band issues should be minimal.
I put together a very well received couple of presentations on fascia and its role in training and recovery in Muscle Imbalances Revealed: Lower Body a few years ago, and it begs to be revisited again, if for nothing more than my presentations on fascia. Additionally, you have other smart guys like Mike Robertson, Bill Hartman, Rick Kaselj and Eric Beard dropping K-bombs left right and center about all things lower body on you, so it’s worth the investment.
A follow-up to this one was a continuation of the fascia thought process in Muscle Imbalances Revealed: Upper Body, which also featured contributions from Tony Gentilcore, Jeff Cubos, Rick Kaselj, and solid info for any trainer, therapist or exercise enthusiast who wants to get completely immersed in technical talk and anatomy.

18 Responses to Some Big Reasons Why Your IT Band Hurts