4 Keys to Recovering from Hip Arthroscopy
Today’s guest post comes from Matt Kelly, a physiotherapist and grad student at McGill university specializing in hockey training, and if you train athletes of any stripe or work with clients who have had any kind of hip issues in the past, I think you’re going to really love digging into this post.
******
Recovering from hip surgery is a long process. Most rehab protocols last approximately 4-6 months. But this is to return to “functional”. If you have specific goals you are looking to return to, the process can be longer.
Unfortunately, hip arthroscopy is becoming a common place in sports such as running, soccer, hockey and basketball. And we are starting to hear about more youth athletes who are having arthroscopic surgery to repair the hip labrum or for FAI.
Two of the more important keys to successfully recover from hip arthroscopy are to restore range of motion and regain strength. I can’t stress enough how important these are. Both will help reduce the risk of further injuries (ie low back pain) and will help you return to full function. But what I want to focus on today are 4 keys to recovery from hip arthroscopy that are often times overlooked.
Work on lumbopelvic control and muscle imbalances early
The issue a lot of people have is that they are unable to control their lumbar spine and pelvis. Having good lumbopelvic control is the foundation to having good hip movements. In the words of Grey Cook “proximal stability for distal mobility”. Imagine trying to shoot a cannon out of a canoe…not very likely to work right? That’s what it’s like trying to move a limb with poor lumbopelvic control.
Lumbopelvic control and muscle imbalances are key factor for hip arthroscopy because poor LP control could be what caused the issue in the first place. Often times, we see people who hang out in an anterior pelvic tilt, which brings the acetabulum and neck of the femur closer together. This will increase the likelihood of pinching the labrum or the bones coming in contact with each other when getting into deep hip flexion, causing bony growth aka FAI. We also see people on the opposite end of the spectrum who sit in a posterior pelvic tilt. This can add more shearing forces on the labrum causing a tear and can stretch on the ligament of the front of the hip (iliofemoral ligament) which can lead to some anterior laxity. If the pelvis is in a poor alignment, it can put undue stress on different or more focal areas of the hip and lead to pathology.
The use of compensatory stabilizers, such as the hip muscles to stabilize the pelvis is often the cause of muscle imbalances. These muscles get tight and change how the femur moves inside the acetabulum. This will also put more stress on one area leading to pathology. So, without changing what is actually causing the issue prior to surgery, we may continue to have similar issues down the road.
Optimize movement patterns
Post-surgery, everything will feel weird and unfamiliar until you normalize your gait pattern. During the early stages of recovery, working on optimizing gait is super important to get back to doing everyday activities. Once walking is normal, then it’s time to clean up everything else.
I think the hip is often overlooked as a potential for injury when assessing movement patterns. We are often busy looking at the shoulder, back and knee, for good reason as these are common places for poor movement and injury. However, by focusing on these areas, we often overlook what is happening at the hip. Let’s take, for example, a lunge.
When assessing the lunge, we often see signs of knee valgus or poor knee control. Most people would say that this poor person is potentially at risk of a knee injury like an ACL tear, which I won’t argue with. But I would also say they are also at risk of impingement of the hip labrum because the hip is flexed, adducted and internally rotated. And for someone post-surgery, this can really irritate any repaired structures in the hip.
This is just one example, but the same can be said for most movements. So key #2 post hip arthroscopy is to optimize movement patterns to 1) fix the potential initial cause 2) avoid irritating post-op tissues. On top of helping you recover, optimizing your movement patterns can help you increase performance by improving movement efficiency.
Dynamic hip stability
The hip cuff plays a huge role in hip stability. Although the hip is inherently a stable joint, Zaffagnini et al. (2016) have shown that the soft tissue surrounding the hip plays an important role in keeping the hip stable. They found that as they removed more soft tissue, femoral head displacement increased. When the hip cuff isn’t working in sync or is weak, we can get micro movements of the femur inside the acetabulum that can put strain on the labrum. But this means that we can train the hip musculature to keep the femoral head centred in the joint.
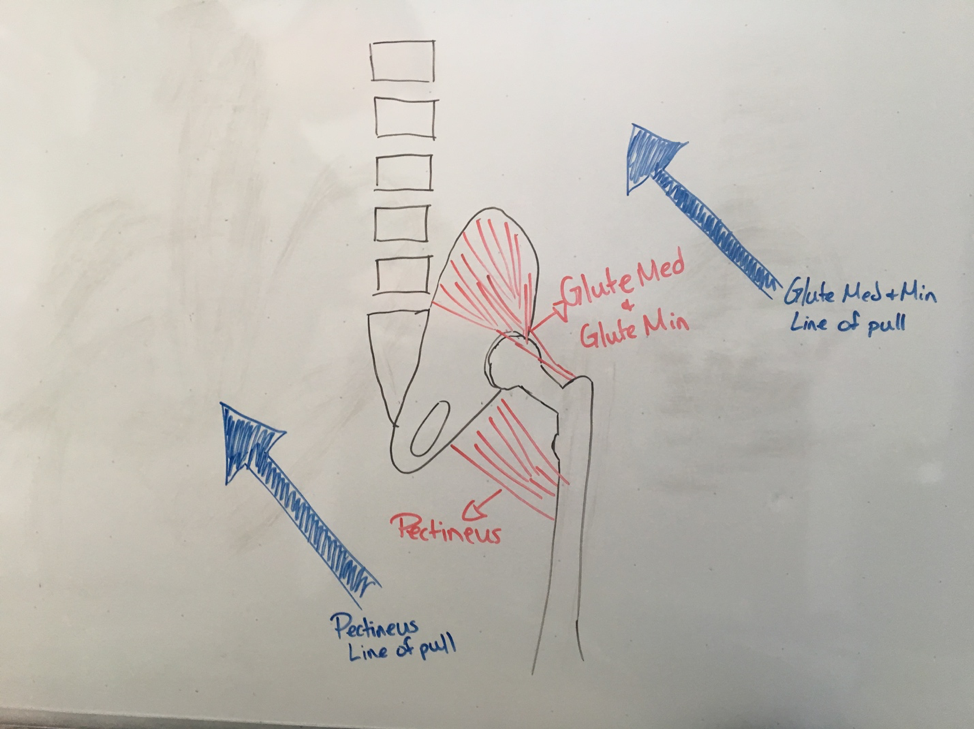
Like the shoulder, we need the smaller hip rotators to centrate the joint while the larger more powerful muscles move the leg. We often focus on glute (med and min) strength which is very important in hip stability, but we often forget that training them to work in sync with other muscles to stabilize the hip is just as important. Single leg training is great for training dynamic hip stability and unstable surface training can add an extra element of difficult, while adding perturbations (manual perturbations or adding another task) are great for reactive stability.
An often-ignored muscle that contributes to the hip cuff is the pectineus. This muscle in the adductor group works synergistically with the deep glute muscles to pull the femur into the socket for increased stability. Adding some groin strengthening can also improve your hip stability.
Bonus – Progressive Overload
In rehab, our focus is primarily on strength and range of motion. Don’t get me wrong, both are very important and set a good foundation to build on, but often times we don’t go any further than that. And this is where I think, as rehabilitation specialists, we do a poor job of preparing our patients for activity. However, we want to make sure to continue to progressively overload and periodize any rehab program. We should be increasing loads, including power exercises, plyometrics, speed and agility with our patients to increase their capacity to handle loads. Obviously, there is a difference in working with a high-level athlete and Joe the barista from Starbucks, but I do believe we should be doing some appropriate variations of these with our patients to help them achieve their goals.
Double Bonus – don’t rush back to your activities
Hip arthroscopy is a very successful procedure and people usually do really well after surgery. But don’t get too excited. The rehab is a process of baby steps and slow progress. The thing is you will likely feel great by month 1 or 2. But I’ll let you in on a little secret: you are not ready to return to activities just yet. Even at month 4, when doctors typically clear people to return to sports/activities, you might not be ready. You can’t just assume that because 4 months have gone by, that you are all set to run with the best of them. Returning to sports/activities also has to be a slow progression of baby steps. Jumping back in with both feet can cause your hip to flare up. You also have to make sure the rest of your body is ready to handle the stresses of whatever it is you are into. Anytime you have a large increase in activity, you put yourself at risk of not only reinjury, but other injuries at well. So make sure you take your time, take small baby steps, and please resist the urge to return early.
Triple (and final) Bonus – Turn injury into an opportunity
(Last one, I promise)
Being injured sucks, straight up. But it can also present as an opportunity. An opportunity for you to work on things you might have on the back burner. For athletes, this could be a skill that you can improve on like stick handling or free throws. Or learn new plays, strategies, watch professional players and learn what they’re doing in different situations. For others, maybe this is an opportunity to read that book you bought last year that’s been doing a great job at filling your bookshelf or learn a new recipe. But make good use of this time by turning this misfortune into an opportunity to grow.
Hip arthroscopy can have really good outcomes. I hope these keys help you be successful in your recovery.
References:
Zaffagnini, S., Signorelli, C., Bonanzinga, T., Lopomo, N., Raggi, F., Roberti Di Sarsina, T., … & Marcacci, M. (2016). Soft tissues contribution to hip joint kinematics and biomechanics. Hip International, 26(1_suppl), S23-S27.
About the Author

Matt Kelly is a former Junior hockey player, who is now a physiotherapist and graduate student in the Ice Hockey Research Lab at McGill University. Matt has worked with athletes of all levels including high school, collegiate and professional. His current interests include hip injuries, in particular hip injuries in hockey players. You can find more from Matt on his blog at www.be-elite.ca, or reach him on Instagram @alwaysbeelite or Twitter @mkellypt.